Looking for resident, faculty and research news for the Department of Anesthesiology at Rush University? Find the latest headlines here.
-
Department NewsImage
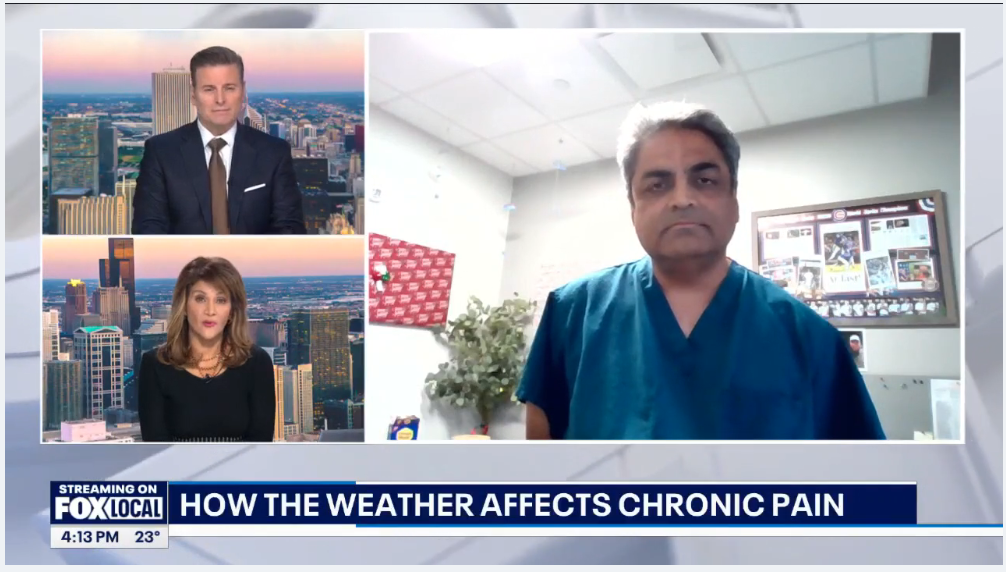
Dr. Sandeep Amin explores the connection between weather changes and chronic pain
If you live with chronic pain, you may notice shifts in the weather before they even appear on the forecast—you can feel them in your body. According to the CDC, emerging “pain forecasts” are now helping predict pain flare-ups by linking weather conditions to symptom changes.
Watch the interview.
Image
Rush celebrates latest endowed faculty appointments: Dr. Asokumar Buvanendran
Rush University honored four esteemed faculty members during a ceremony on June 26, recognizing their appointments to endowed positions. Endowed faculty appointments, such as Dr. Buvanendran's, many made possible by the generosity of philanthropic partners, are the university’s highest honor and demonstrate confidence in and commitment to Rush’s future.
“It is my honor to recognize our donors' generosity and celebrate the exceptional faculty members whose leadership and contributions are shaping the future of health care — for learners, patients and communities alike.” said Julie Hoff, PhD, RN, FNAP, FAAN, provost of Rush University
The Anthony D. Ivankovich, MD, Chair of Anesthesiology was established by faculty, former students and friends of Ivankovich to recognize his achievements and contributions to Rush and the field of anesthesiology. It provides support for basic research and educational initiatives.
Buvanendran, chairperson of the Department of Anesthesiology at Rush University Medical Center, specializes in pain medicine. He knows Ivankovich personally and has worked to reinforce the characteristics the chair’s namesake instilled in the department.
“It’s an outstanding honor to continue Dr. Ivankovich’s legacy of producing clinical excellence for patients, not only in the anesthesia field but also in pain medicine,” Buvanendran said. “I am tremendously proud of the trust the university puts in my capabilities, including with this endowed chair.”
Read the full article.
Image
Congratulations to Jennifer Huh, MD Recipient of the 2025 Katalin Selmeczi, MD & Curt J Stokes, III MD Memorial Award!
This award is given to the graduating resident in Anesthesiology who embodies the spirit, humanism, devotion, courage, and work ethic exemplified by Katalin Selmeczi, MD and Curt J. Stokes, MD.
And
Congratulations to Elizabeth Morin, DO Recipient of the 2025 Robert D. Dripps, MD Memorial Award!
The award is presented annually to the outstanding graduate resident in Anesthesiology.
Image
Interview with the 2025 Distinguished Service Award Recipient: Dr. Asokumar Buvanendran
Congratulation to Dr. Buvanendran on his award. Former American Society of Regional Anesthesia and Pain Medicine (ASRA Pain Medicine) President Asokumar Buvanendran, MD, has been selected as a recipient of the 2025 Distinguished Service Award (DSA) in recognition of his outstanding contributions to regional anesthesiology and pain medicine.
A national leader in pain management, he has played a pivotal role in advancing multimodal analgesia protocols (opioid sparing), particularly in orthopedic surgery. His current research, funded by National Institutes of Health (NIH) and Department of Defense grants, explores pain mechanisms, alternatives to opioids, and the transition from acute to chronic pain. A key focus is preventing chronic pain after surgery, which helps reduce opioid use in patients.
The DSA celebrates individuals who have made significant contributions to regional anesthesiology and/or pain medicine through scholarly activities, clinical teaching, and service to ASRA Pain Medicine or the scientific and medical specialties practiced by ASRA Pain Medicine members. Dr. Buvanendran will be presented with the award at the 50th Annual Regional Anesthesiology and Acute Pain Medicine Meeting, held May 1-3, in Orlando, FL.
Image
Congratulations to Dr. Behnoosh Shayegan, MD on Receiving the Rush Good Catch Award
Dr. Shayegan, noticed a suspicious discrepancy in a charted information for a weight based medication on a pediatric patient. After investigating she immediately made appropriate corrections avoiding possible issues. We applaud Dr. Shayegan for her diligent attention to detail.
Image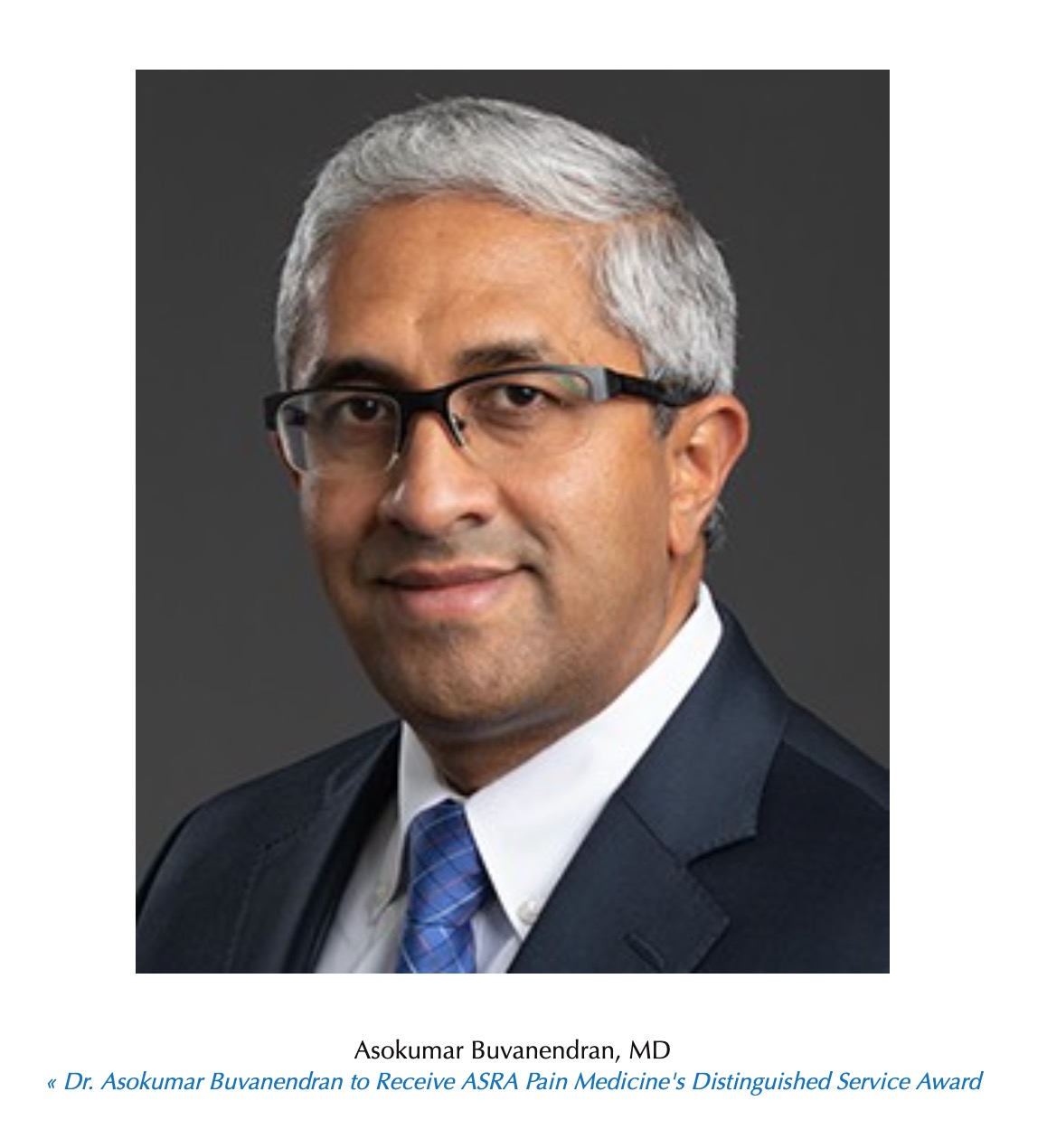
Dr. Asokumar Buvanendran to Receive ASRA Pain Medicine's Distinguished Service Award
Former American Society of Regional Anesthesia and Pain Medicine (ASRA Pain Medicine) President Asokumar Buvanendran, MD, has been selected as a recipient of the 2025 Distinguished Service Award (DSA) in recognition of his outstanding contributions to regional anesthesiology and pain medicine.
A national leader in pain management, he has played a pivotal role in advancing multimodal analgesia protocols (opioid sparing), particularly in orthopedic surgery. His current research, funded by NIH and Department of Defense grants, explores pain mechanisms, alternatives to opioids, and the transition from acute to chronic pain. A key focus is preventing chronic pain after surgery, which helps reduce opioid use in patients.
Image
The Department of Anesthesiology Leadership Award was presented to Dr. Christopher O’Connor for his exemplary service, dedication to patient safety, and exceptional leadership.
Dr. O’Connor joined Rush in 1991 after completing a medical residency, an infectious diseases fellowship, an anesthesia residency, and a cardiac anesthesia fellowship. Over the past four decades, he has been a cornerstone of our department, combining unmatched clinical expertise with steadfast leadership. His dedication to education, patient safety, and innovation has profoundly shaped the field of anesthesiology. As a master teacher of ABA exams, he has mentored hundreds of residents, leaving a lasting impact on their careers and the profession
Image
The Clinical Excellence Award was awarded to Dr. Timothy R. Lubenow, a pioneer in pain management, in recognition of his extraordinary contributions to pain medicine and patient care.
=Dr. Lubenow has dedicated four decades to advancing the field of pain management since joining the department in 1987. Nationally recognized for his pioneering interventional techniques, groundbreaking research, and mentorship of countless trainees and colleagues, his work has earned him a reputation as one of the foremost experts in pain medicine in the country. His contributions have profoundly improved the lives of patients and inspired the next generation of professionals in the field.=
Image Image
Image
Congratulations to Dr. Denis Snegovskikh, recipient of the Outstanding Educator of the Year 2024 award.
The Educator of the Year Award is selected through a voting process by the residents and recognizes a faculty member who has made significant and positive impacts on the education of residents. Dr. Snegovskikh’s dedication to teaching and his ability to foster a supportive and enriching learning environment have made him an invaluable mentor to our department’s trainees.
Congratulations to Dr. Graham Lubinsky, awarded the Outstanding Mentor of the Year 2024.
This award, voted on by residents, recognizes exceptional attending anesthesiologists who have demonstrated a deep commitment to mentoring the next generation of anesthesia professionals. Dr. Lubinsky’s guidance and support have left a lasting impression on his mentees, empowering them to grow and succeed in their careers.
Image
Congratulations to Michael Nemsick, MD for scoring in the top 10 percent among those who took the ABA Basic Examination this June 2024.
Image
Congratulations to Jessica Richelieu, MD Recipient of the 2024 Katalin Selmeczi, MD & Curt J Stokes, III MD Memorial Award!
This award is given to the graduating resident in Anesthesiology who embodies the spirit, humanism, devotion, courage, and work ethic exemplified by Katalin Selmeczi, MD and Curt J. Stokes, MD.
Image
Congratulations to Theodore Stewart-Hester, DO, Recipient of the 2024 Robert D. Dripps, MD Memorial Award!
The award is presented annually to the outstanding graduate resident in Anesthesiology.
Image
Outstanding Educator of the Year
Congratulations to Sarah Cocoma, MD, awarded the Outstanding Educator of the Year 2023, voted annually by the residents in the Department of Anesthesiology.
Image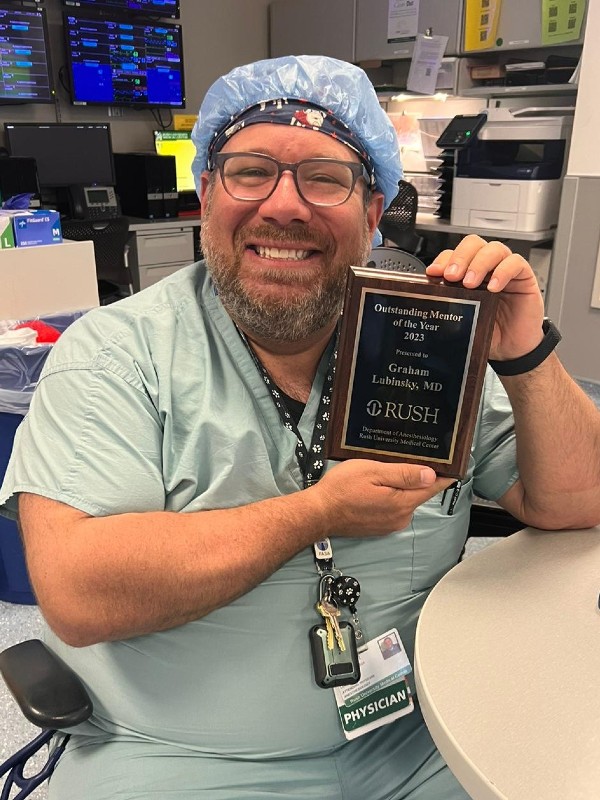
Outstanding Mentor of the Year
Congratulations to Graham Lubinsky, MD, awarded the Outstanding Mentor of the Year 2023, voted annually by the residents in the Department of Anesthesiology.
Image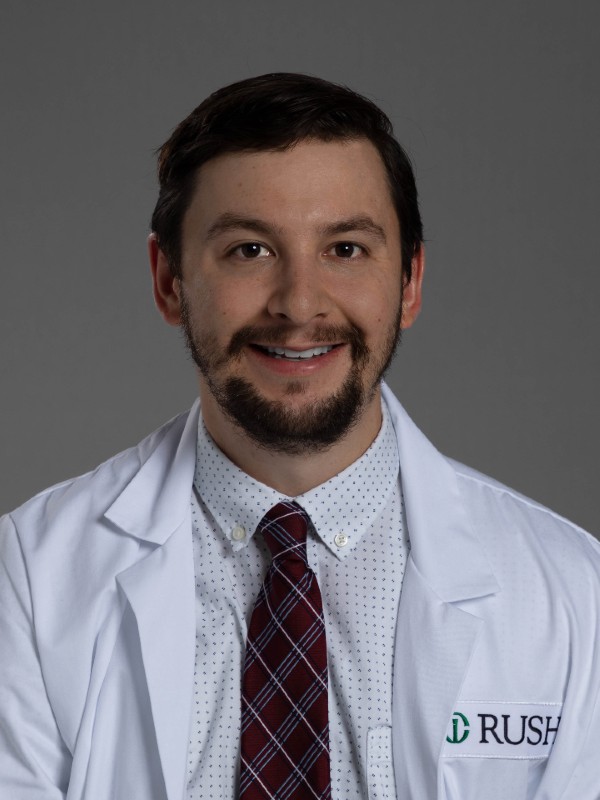
Congratulations to Christopher Reglen, MD for scoring in the top 10 percent among those who took the ABA Basic Examination this June 2023.

Congratulations to Dr. Sarah M. Cocoma, MD on being named the non-surgical attending of the Year!
Dr. Cocoma, MD is the director of the critical care section and chair of the clinical competency committee. Dr. Cocoma, MD has previously received the attending of the year, the non-surgical attending of the year and “Hero of the Heart” award. She will be receiving the award at the General Surgery Residency Graduation, June 23, 2023. The department congratulates her on consistently outstanding performance and commitment to Rush community values.
Image
Congratulations to Dr. Lubenow, MD on his Lifetime Achievement Award
Dr. Timothy Lubenow, Professor, Rush Medical College, Director of Postoperative Analgesia Services, Director of Rush University Pain Center and Director of Pain Management, Rush University Medical center will be presented with a Lifetime Achievement award at the American Society of Pain and Neuroscience (ASPN) conference this summer at the awards symposium. The department of Anesthesiology here at Rush, is honored to have Dr. Lubenow part of the department for over 20 years and congratulate him on his most deserving lifetime achievement award.
Image

Congratulations to Jared Konner, DO Recipient of the 2023 Katalin Selmeczi, MD & Curt J Stokes, III MD Memorial Award
This award is given to the graduating resident in Anesthesiology who embodies the spirit, humanism, devotion, courage, and work ethic exemplified by Katalin Selmeczi, MD and Curt J. Stokes, MD.
Image
Congratulations to Sara Izzo, DO, Recipient of the 2023 Robert D. Dripps, MD Memorial Award
The award is presented annually to the outstanding graduate resident in Anesthesiology.
Image
Lindsay’s Story: African Primate Rehab Specialist Gets Rush and University Pain Center care for Rare Conditions
Lindsay Maess fulfilled a lifelong passion by working with monkeys, chimps and gorillas at US zoos and often returning to Africa for field research at the Pandrillus conservation organization and sanctuary for orphaned chimpanzees and endangered drill monkeys in Nigeria.
Life in the jungle can pose dangers we don’t face in the Western world. When Lindsay came down with malaria, it set her on a path to severe neurological issues, pain and trauma that took so many years of her life and, if it weren’t for her team of physicians at Rush, could have ended her dream forever.
In April of 2016, Lindsay tested positive for a parasitic infection — Plasmodium falciparum.
The day after she began her third round of medication, Lindsay developed the worst headache of her life. The next few days brought shooting pain through her whole head, fever and bleeding sores all over her face. She felt like electricity was running through her tongue, lips, face and ears.
The pain spread to her shoulders, spine and left arm. She felt dizzy and confused, like she was intoxicated.
By the time Lindsay came to Rush in January of 2019, her life had completely changed. She could barely swallow, talk or be social anymore — much less continue her life’s work with primates.“To get through those years before coming to Rush, I didn’t want to live through it,” Lindsay says. “The pain and vertigo were so intense, and I thought there was no way I could keep going like this.”
At Rush, she would finally get relief, not only from one doctor, but from a community of physicians that worked together to address all her medical concerns.
Lindsay was referred to Dr. Ryan Smith, MD, a facial plastic surgeon at Rush who specializes in treating facial nerve disorders. Assuring he would do whatever it took to help, he worked to tailor her treatment.Lindsay also worked with Dr. Sandeep Amin, MD, a pain management physician at Rush and University Pain Centers (UPC), to further treat her nerve pain and migraine. “Her nervous system was in hyper-drive mode when I first saw her, accounting for her facial issues, pain, headaches and difficulty swallowing,” Dr. Amin says.
To treat these issues, he used ultrasound imaging as a guide to place several nerve blocks, injecting anesthesia into specific nerves in Lindsay’s head and neck. “It’s almost like resetting the neurologic system and bringing it into normal drive mode,” Dr. Amin says.
“Dr. Smith and Amin, what’s so special about them is that they’ll sit and listen,” Lindsay says. “They’ve been so patient and persistent with me. Dr. Smith has probably missed lunch hours just from answering my many questions and letting me express everything I wanted to say. And Dr. Amin has been relentless at peeling back and treating the layers of my pain with compassion.”
Image
Dr. Tolga Suvar, MD has been appointed Director of Cancer Pain Management
The department is proud to announce that Dr. Tolga Suvar, MD has been appointed Director of Cancer Pain Management here at the Rush University Medical Center. Dr. Suvar, after residency at the University of Arkansas for Medical Sciences completed his fellowship in Pain Medicine, here at Rush, after which we were delighted that he chose to join our department. Dr. Suvar’s expertise with chronic pain was refined with his tenure as a pain specialist at the Rush University Pain Center (UPC). We congratulate Dr. Suvar on this prestigious appointment and look forward to his continued success.

Outstanding Educator of the Year
Congratulations to Graham Lubinsky, MD, awarded the Outstanding Educator of the Year 2022, voted annually by the residents in the Department of Anesthesiology.

Outstanding Mentor of the Year
Congratulations to Lisa Solomon, DO, awarded the Outstanding Mentor of the Year 2022, voted annually by the residents in the Department of Anesthesiology.
Image
RUMC Department of Anesthesiology Annual Holiday Party is Back!
The Department of Anesthesiology hosted their annual holiday party January 2023 at the Shedd Aquarium, just off the lakefront in downtown Chicago. It was a fun-filled night of laughter, a delicious dinner, decadent desserts and dancing.
To view a slideshow of photos from this event click on the following link: https://drive.google.com/file/d/1MCYFx8bnHQLPQ3bXQAvN84Mgds1pwnHr/view?usp=sharing
Image
Congratulations to Dr. Bhatia on her invitation to become an ABA Examiner
Dr. Alisha Bhatia, MD, FASA was invited by the American Board of Anesthesiology (ABA) as an examiner for the applied ABA exam, which evaluates the ability to communicate professionally while probing technical competency, judgment, adaptability, and organization. The department is honored that Dr. Bhatia was selected for such an important position, as ABA certification assures that anesthesiologists have the knowledge and skills to deliver the highest quality care. Dr. Bhatia's anesthesiology residency was conducted at John H. Stroger, Jr. Hospital of Cook County with additional education at Brigham & Women’s Hospital for her Critical Care Medicine fellowship. Dr. Bhatia has board certifications in Critical Care Medicine and Anesthesiology.
DEI Award
Congratulations to Aaron Varatharajan, MD, Bishir Clayton MD, and Lisa P. Solomon DO, FASA recipients of the ISA and ASA diversity, equity and inclusion grants.
Image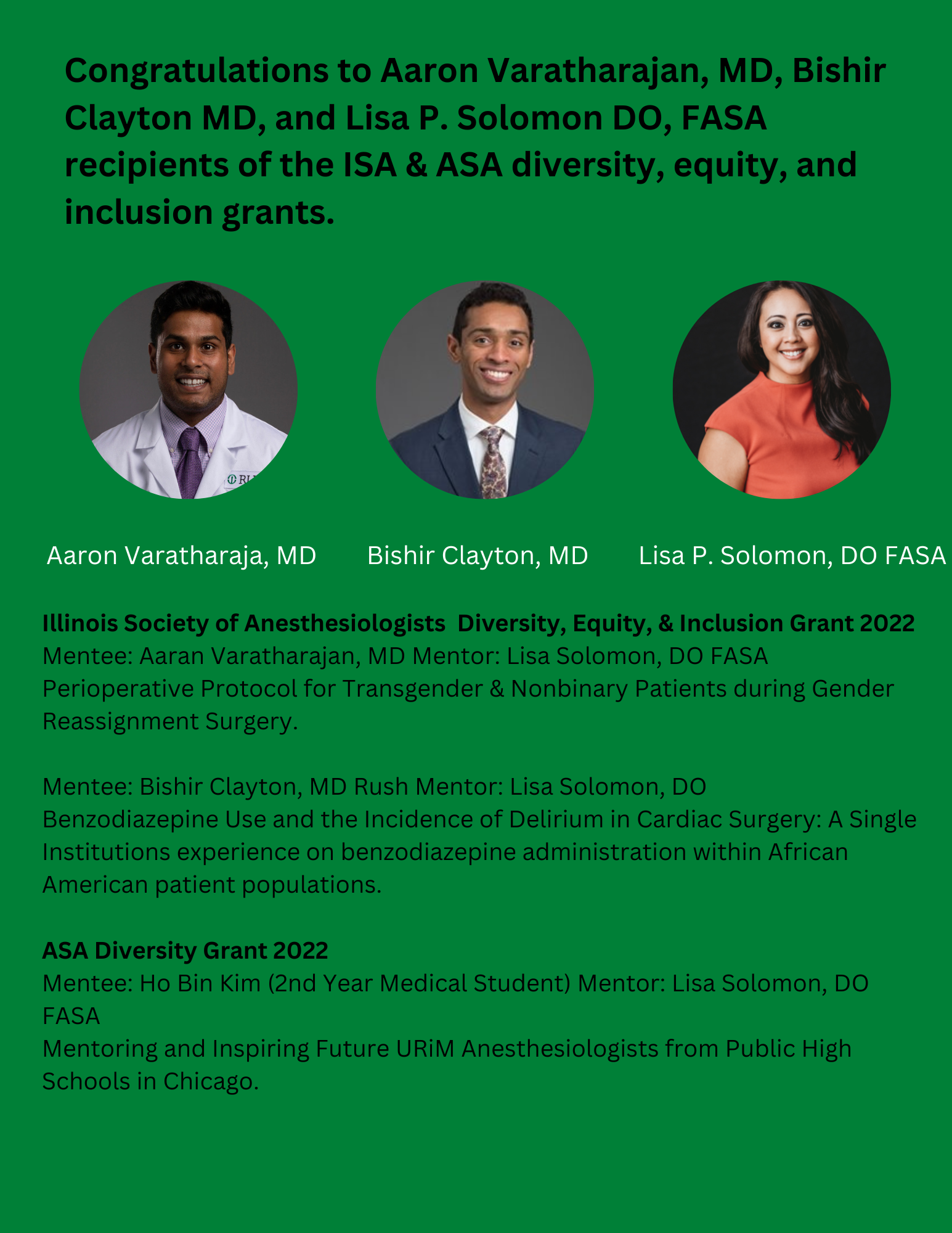
Congratulations to Andrew Keeney, DO and Theodore J. Jeske, DO for scoring in the top 10 percent among those who took the ABA Basic Examination this June 2022.
Image
Pictured: Andrew Keeney, DO.
Image
Pictured: Theodore J. Jeske, DO
Image
Vikash J. Patel, DO Recipient of the 2022 Robert D. Dripps, MD Memorial Award
The award is presented annually to the outstanding graduate resident in Anesthesiology.
Image
Haley M. Wardrip, MD Recipient of the 2022 Katalin Selmeczi, MD & Curt J Stokes, III MD Memorial Award
This award is given to the graduating resident in Anesthesiology who embodies the spirit, humanism, devotion, courage, and work ethic exemplified by Katalin Selmeczi, MD and Curt J. Stokes, MD.
Image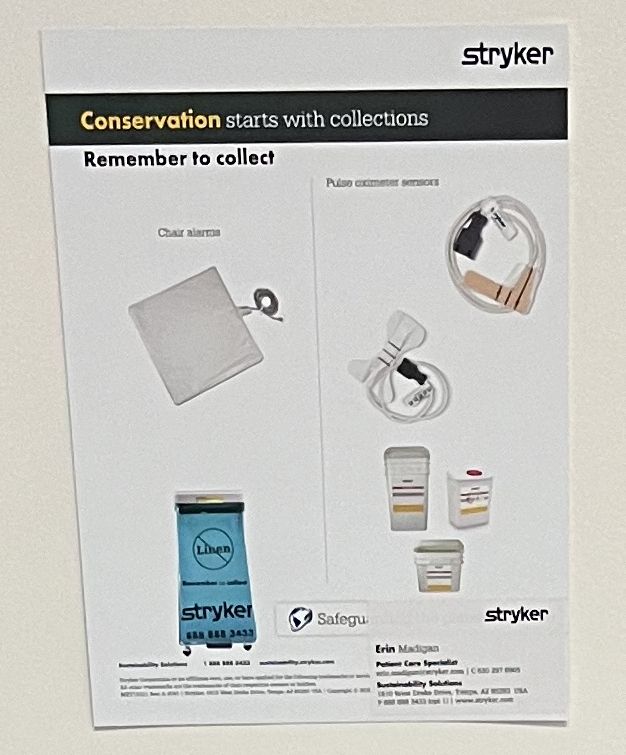
Environmental Excellence Award
Rush University Medical Center was recently awarded a GOLD Award by Stryker Sustainability Solution's team for their efforts to reduce waste. In 2021 Rush diverted 10,000 pounds of waste. We are continuing to work toward more sustainable process, workflows, and operations in the coming years and appreciate the efforts of all the Rush teams.
Image Image
Image
Dr. Solomon interviewed on Millennials access to accurate medical information
A new study shows 37% of millennials, or those ages 25 to 34 years old, do not trust their health care providers.
The high prevalence of medical misinformation available for all ages has led to a greater push to educate the public. The U.S. Surgeon General declared public health misinformation an “urgent threat to public health” in October 2021.
A recent study from Harmony Healthcare IT indicates that 69% of its millennial respondents searched online for health and medical advice instead of going to the doctor. In addition, 25% of these respondents reported they had also trusted online information to diagnose their symptoms accurately. This can come at a dangerous health risk as over 70% of people have been exposed to medical or health-related misinformation.
While information is instantaneous and accessible for those with internet access, the problem with online medical information is the rapid exchange and spread of information that may not be credible, which leads to further confusion. In addition, patients may misdiagnose their medical issue, request unnecessary tests or delay treatment.
"As a board-certified cardiac anesthesiologist, I understand that physicians have the knowledge needed to diagnose and treat medical conditions and online sources do not replace the 12-14 years of medical school and residency. But physicians can do more to address medical misinformation."
It is imperative that everyone, not just millennials, are extremely cautious of relying on unvetted online medical information. Misinformation is dangerous.
Image
Student National Medical Association (SNMA) 2022
This year the SNMA was hosted in Orland, FL and the department was proud to have Dr. Sanguino represent Rush University Medical Center and the Department of Anesthesiology. Medical students of all education levels attend the SNMA's Annual Medical Education Conference, which is consistently the largest gathering of underrepresented minority medical students in the nation.
“This was my first time attending the SNMA conference. During this conference I was extremely happy to meet many people from various ethnic backgrounds from high school all the way to medical school inquiring about Rush and Anesthesiology in particular. As a first generation Hispanic in the US and first physician in my family, I believe it is very important to continue to encourage young, underrepresented students to pursue a career in medicine and to show them that it is not impossible for people with a different ethnic and cultural heritage to become a physician."
- Luis Sanguino, MDImage Image
Image Image
Image
Dr. Jay L. Shils, PhD, D. ABNM, FASNM elected to chairperson of the of the American Board of Neurophysiological Monitoring (ABNM)
The department of Anesthesiology would like to congratulate Dr. Shils on his election as Chairman of the American Board of Neurophysiological Monitoring. Additionally, he is the Director of Neurophysiological Intraoperative Monitoring as well as a Full Professor in the department of Anesthesiology at Rush.
Dr. Shils is an expert in Neuromodulation, Microelectrode recording, and Intraoperative Neurophysiological Monitoring techniques and applications.Image
Rush Residents Drs. Petravick and Desai featured on ASA Residents in a Room podcast - Discussing Technological Changes
Dr. Dillon Tinevez discusses how technological changes have impacted the practice of anesthesiology with fellow residents Drs. Shyam Desai, Mike Petravick, Janhavi Dhargalkar, Artush Grigoryan and Kannan Aravagiri. From apps and wearable technology to learning curves and evolving skill sets, guests consider the many ways technology has shaped anesthesiologists’ practices, skills, and experiences.
Listen to Residents in a Room Episode 36: Past to Present – Technological Changes
Link to Podcast on ASA website
Image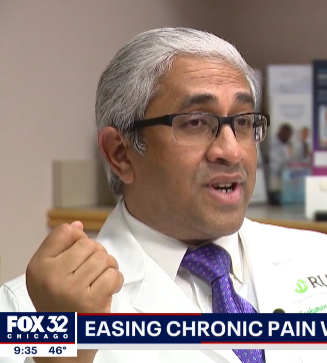
Dr. Buvanendran on FOX 32 - Cutting Edge Therapies for Chronic Pain Being Developed at Rush
Cutting edge therapies for chronic pain are being developed in Chicago at Rush hospital.
“The incidence of chronic pain is significant," said Dr. Asokumar Buvanendran the Anesthesiology Department Chair at Rush University Medical Center. "In fact, it is much more than hypertension and diabetes combined," he added.
Rush is partnering with the National Institute of Health to identify where chronic pain originates and who is most susceptible to developing it.
They are using MRI scans of the brain to get their results.
"Traditionally, pain is reported by the patient, but we can actually see documented evidence now in the brain of the circuits that light up with chronic pain. So that's a really exciting and new field that's developed over the years," said Dr. Buvanendran
Instead of prescribing opioids, doctors are now able to insert electrodes surgically into the spine to stop pain signals before they reach the brain and trigger discomfort. "So if you're able to interrupt the signals in the process, you naturally can cut down the pain signals going to the brain, and therefore you decrease the pain perception," said Dr. Buvanendran.Image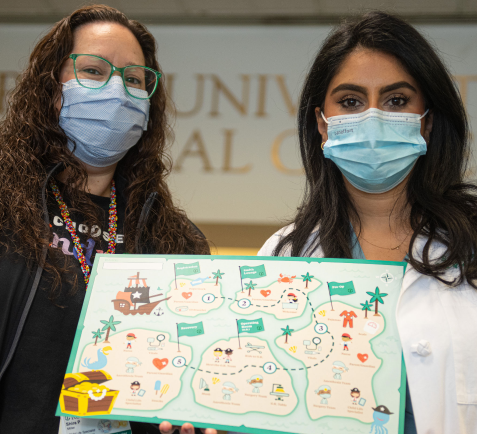
Helping Kids Navigate Surgery
Going into surgery is nerve-racking for anyone, but it can be especially frightening for children. Rush University Children’s Hospital has a new tool that is helping Rush’s youngest patients better understand their surgery experience and take on an active role in their care — all while having fun.
Behnoosh Shayegan, MD, director of pediatric anesthesiology, first got the idea for a tool like this while completing her anesthesiology fellowship. She witnessed what a difficult and stressful time this could be for children and dreamed of creating something fun and interactive that could help ease the anxiety of patients going through the surgical process.
Dr. Shayegan teamed up with Shira Miller, MS, CCLS, manager of child life and creative arts therapies, and the two thought through every stage of a patients’ journey into surgery from the moment they walk through the doors to discharge. The treasure map has been a longtime vision of Shayegan’s.
“I wanted to create an interactive tool that puts the patients themselves in charge of their care,” Dr. Shayegan says. “When kids are involved in something that they’re usually scared of, they tend to react more positively.”
As patients make their way through the day of surgery and conquer each island on the treasure map, they get a sticker to mark the completion of another step. When the young explorers finally land at Recovery Island, aka the recovery room, they have reached the treasure and are able to collect a prize from a treasure box which includes small, age-appropriate toys.Image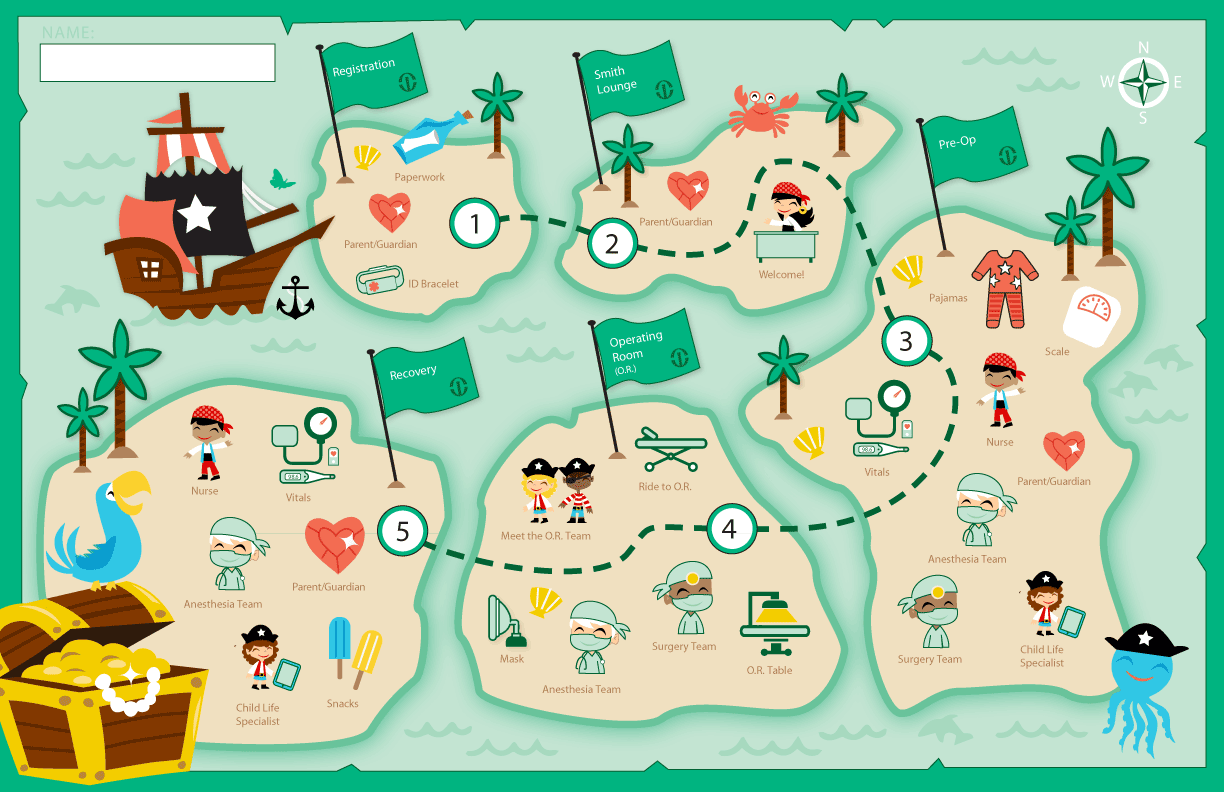 Image
Image
Congratulations to Dr. Behnoosh Shayegan on her Promotion to Associate Professor!
It is with great please that we congratulate Dr. Shayegan, MD on her promotion within Rush Medical College to the rank of Associate Professor in the Department of Anesthesiology. Dr. Shayegan’s work as an anesthesiologist and as the Director of Pediatric Anesthesiology has brough her both academic and professional accolades, and we wish her continued success.
Image
Congratulations to Dr. Rajagopal on his promotion to Associate Professor
It is with great pleasure that we wish to announce the promotion of Dr. Arvind Rajagopal, MD, MPH, currently the director of the Anesthesiology residency program, to the rank of Associate Professor. We are grateful for the many years of dedication he has shown to the anesthesiology department, and we hope for many more.
Image Image
Image
Congratulations to Drs. Amin and Birmingham on their Promotion to Associate Professor
The Anesthesiology department would like to thank Dr. Sandeep Amin, MD, Director of Anesthesia Rush Oak Park Hospital, Medical director of the Rush Oak Park Pain Clinic, as well as Dr. Brain Birmingham, MD, Director Cardiac Anesthesiology & Liver Transplant Anesthesiology, for their contributions to the department and congratulate them on their well deserved promotion to Associate Professor.
Image
Guest Speaker William McDade, MD, PhD
Dr. William McDade recently presented Diversity and Inclusion in Graduate Medical Education at the Department of Anesthesiology's weekly Grand Rounds.
William McDade, MD, PhD is Chief Diversity, Equity and Inclusion Officer for the Accreditation Council for Graduate Medical Education. Dr. McDade was recently appointed Adjunct Professor in the Department of Anesthesiology at Rush University Medical Center. He has been Chief Academic Officer/EVP for the Ochsner Health System, Professor and Deputy Provost at the University of Chicago, and Associate Dean at the Pritzker School of Medicine. He has served on the executive committee of the Joint Commission Board and has served on boards for the AMA, NBME, and ACGME. He has been a President and Board Chair of local and state medical societies in Illinois and Chair of the National Medical Association’s Anesthesiology Section and the AMA’s Council on Medical Education. He is a board-certified Anesthesiologist having graduated from the Prizker School Medical Scientist Training Program, earning a PhD in Biophysics and Theoretical Biology. He completed an internal medicine internship at UChicago and his anesthesiology residency at the Massachusetts General Hospita.
Image
Lisa Solomon, DO
Dr. Lisa Solomon joins Rush University Medical Center as an assistant professor in the Department of Anesthesiology. She received her D.O at Chicago College of Osteopathic Medicine and completed her fellowship in Cardiothoracic Anesthesia at Loyola University. Recently, Dr. Solomon was published in ASA Monitor with the topic of “Health Literacy in Anesthesia: Moving the Needle in Health Equity.” To view the article, please click on the following link https://pubs.asahq.org/monitor/article/85/8/27/116105/Health-Literacy-in-Anesthesia-Moving-the-Needle-in
Image
Class of 2021 Resident and Farewell Dinner
On Saturday, June 5th, 2021, the Department of Anesthesiology hosted a small gathering to celebrate the Class of 2021 Anesthesiology Residents, Pain Medicine Fellows, and Regional Anesthesia Fellow. The event took place at Gibsons Bar and Steakhouse in downtown Chicago. Smiles and laughter filled the air as we all reflected on their past experiences and accomplishments while at Rush University Medical Center.
To view photos from this event and other departmental Instagram posts click on the following link: https://www.instagram.com/p/CT5etPOPu9i/?utm_medium=share_sheet
Image
Jordan Schell, MD awarded the Robert D. Dripps, MD Memorial Award
The award is presented annually to the outstanding graduate resident in Anesthesiology.
Image
Teuta Marsic, MD awarded the Katalin Selmeczi, MD & Curt J. Stokes, III, MD Memorial Award
The award is given to the graduating resident who embodies the spirit, humanism, devotion, courage, and work ethic exemplified by Katalin Selmeczi, MD and Curt J. Stokes, MD.
Image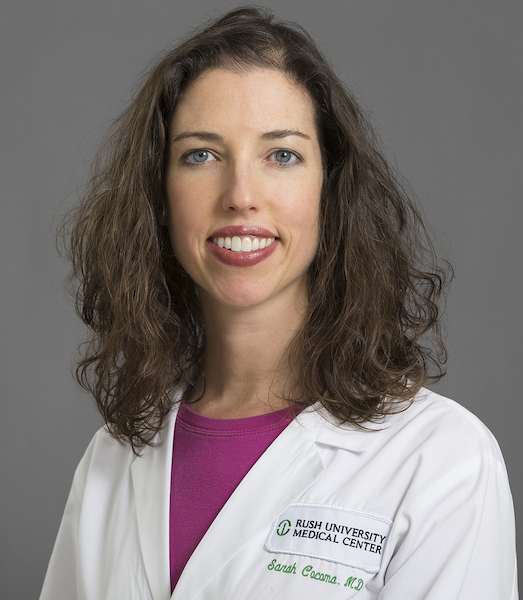
Dr. Cocoma awarded Non-Surgical Attending of the Year
Rush University Medical Center surgical residents have selected Dr. Sarah Cocoma as this years "Non-Surgical Attending of the Year". The anesthesiology department hardily congratulates Dr. Cocoma on wining this prestigious award. The award was presented to Dr. Cocoma at the surgical residents' virtual graduation on June 26th, 2021.
Image
Darren Gorman, MD, nominated for Hero of the Heart award
Image
Darren Gorman, an anesthesiology resident, was nominated for the Hero of the Heart award on June 28, 2021 by the chaplain, Flora Tang. It was for his involvement with an extubation in the AICU. Flora said,
"I was the on-call chaplain on Thursday, 6/24/2021 evening, when Darren paged me to support the family of a patient on 10W who was being compassionately extubated. I witnessed how Darren supported the emotional needs of different members of the family while patiently answering medical questions and suggesting that they do not witness the extubation, while going out of his way to care for the family’s spiritual needs as well. I was able to feel how much care there was in the brief encounter for the grieving family’s wellbeing.
May you continue to be a source of both healing and inspiration to the entire Rush University Medical Center. You are an exemplary credit to your profession and a true Hero of the Heart."
2021 ASA Resident Ambassador
Congratulations to Ryan Kuta, who was selected as a member of the 2021 American Society of Anesthesiologists Resident Experience team. Ryan will work with nine other peers across the country to create a new space for thoughtful, candid discussion in a private online environment built by and for residents.
Image
2021 ASA “Best of Abstracts"
Congratulation to Dr. Vaskar Das on being awarded the American Society of Anesthesiologist (ASA) 2021 conference “Best of Abstracts: Basic Science" for his abstract "Effect of Opioid and Ampa Antagonists on (2r,6r)-HNK (Hydroxynorketamine) Anti-hyperalgesic Activity" at ANESTHESIOLOGY 2021 Annual Meeting to be held in San Diego, California on Sunday, October 10th, 2021
Image
Pillsbury Trust Award
Congratulations to Luis Sanguino, one of this year’s recipients of the Pillsbury Trust Award. The Pillsbury Hospital Residents Trust was established to provide financial aid to residents and fellows during their advanced training in the various fields of medicine and surgery.
Image
A Holiday Thanks to the Pediatric Anesthesiology Team
Child Life Services sends a huge shoutout to this team from University Anesthesiologists seen in the photo, who generously collected and donated toys for the pediatric patients in Rush University Children's Hospital this holiday season. This donation was organized by Behnoosh Shayegan, MD, director of pediatric anesthesia, and Shira Miller, MS, CCLS, manager, Child Life.
Image
2020 Schweppe Foundation Grant Award
Congratulation to Dr. Vaskar Das on the 2020 Schweppe Foundation Grant and Armour pilot grants (Ketamine Metabolite, (2R, 6R) - Hydroxynorketamine as an Alternative Analgesic Target in Low Back Pain, Evaluation of Direct and Indirect Analgesic Efficacy in a Murine Low Back Pain Model), he was recently selected using an NIH-style peer-review panel comprised of Rush research faculty members. These grants will allow development of preliminary data to enable the investigators to be competitive for future federal or private funding. Thank you to the review panel members and congratulations to the awardees! Dr. Das is the principal investigator on this award grant in collaboration with Dr. Asokumar Buvanendran and Dr. Robert McCarthy (Department of Anesthesiology).
Click here to view award recipients.
Image
Maiko Yamashita, CRNA winner of the Ellen Elpern Voice of the APRN award for 2020
Maiko Yamashita, CRNA has been selected as the winner of the Ellen Elpern Voice of the APRN award for 2020. This is the first time that a CRNA has been awarded this Rush system-wide recognition for excellence in practice, mentoring and leadership.
Congratulations Maiko on this outstanding achievement!!
-
Faculty News
Raj and Dr. Buvanendran Propose National Opioid Safety Fund and Database; Plugs Holes in Bill Recently Passed by Congress
The proposal would create a national Prescription Drug Monitoring Program by turning the existing state-by-state efforts into an interactive, nationwide network. “Our state and local governments need a full partner in their struggles to deal with this growing crisis, including the resources to end multiple prescriptions and provide the effective addiction treatment that people need,” Raja Krishnamoorthi (D-Schaumburg) said.
Click for the original article
Image
Get your elective surgeries in now, some doctors say
As elective surgeries get the green light to resume, some patients may have concerns about getting surgery during the COVID-19 pandemic. As elective surgeries begin to resume, some doctors are recommending their patients have surgery now in case there is another spike in COVID cases. Parag Patel, MD, an anesthesiologist at Rush University Medical Center stated, “We keep up-to-date with all the most current guidelines put out there by the Department of Public Health as well as the CDC.”
For elective surgeries, hospitals are implementing new protocols to keep everyone safe.
Image
“We do a screening out front before they come in. Check their temperatures. Check for any symptoms. We are testing all of our patients for COVID before they come in for surgery,” said Dr. Patel.
Image
Pain Management during the COVID-19 Pandemic
Dr. Buvanendran and colleagues have come together to address pain management and care during the COVID-19 Pandemic with a recent publication:
Chronic pain is the leading cause of disability in the world, is associated with multiple psychiatric co-morbidities, and has been causally linked for the opioid crisis. Access to pain treatment has been called a fundamental human right by numerous organizations. The current COVID-19 pandemic has strained medical resources, creating a dilemma for physicians charged with a responsibility to limit spread of the contagion, and their responsibility to treat the patients they are entrusted to care for. To address these issues, an expert panel was convened that included pain management experts from the military, Veterans Health Administration, and academia.
Image
Dr. Christopher O'Connor: Treating COVID-19 "like nothing I've ever seen" Article in the Daily Herald
This week started with O'Connor manning a newly outfitted intensive care unit specially designed to treat COVID-19 patients. "A COVID patient who has viral pneumonia, they are a different animal completely," says O'Connor, a member of the American Society of Anesthesiologists in Schaumburg. "They are more challenging to ventilate."
Starting work in a new ICU, similar to a Mobile Army Surgical Hospital (MASH) used during wars with professionals spanning medical fields, resulted in O'Connor working with people for the first time. People had "some trepidation about what would happen, but we all came together. I was proud people came together very quickly as a team," he says.The American Society of Anesthesiologists has issued statements on the complications of using one ventilator for multiple patients and converting anesthesia gas machines to ICU ventilators, and a list of resources for anesthesiologists and health care professionals.
Image
Dr. Vaskar Das, PhD awarded the 2021 Cohn Fellowship
Dr. Vaskar Das, Ph.D., joined Rush University Medical Center as an instructor and postdoctoral fellow in the Department of Anesthesiology and currently continuing his research in collaboration with Dr. Asokumar Buvanendran MD, Dr. Jeffrey Kroin, Ph.D. and Robert J McCarthy, Pharm D. His research has broadly focused on new non-opioid treatments for acute and chronic pain mechanism by following (i) the key energy sensor AMPK (adenosine mono-phosphate activated kinase) & (ii) the analgesic effect of the ketamine metabolite, (2R,6R)-hydroxynorketamine that could be the unique targets in pain therapeutics which could replace opioids. His Cohn research will expand to assess the analgesic efficiency and mechanisms of AMPK activators providing a much needed pharmacological understanding of AMPK activators for low back pain, and post-surgical pain. This project will establish a framework for the rational understanding of pain and will help to evaluate AMPK activators for improving pain management and replacing opioids.
Image
Dr. Timothy Lubenow featured in Chicago Magazine's 2020 List of Top Doctors
356 physicians in more than 60 specialties have been chosen by their peers as the finest in the Chicago area. Congratulations to Dr. Lubenow for achieving this recognition.
Asokumar Buvanandran, MD, Recognized by HHS for Contributions to Acute and Chronic Pain
Image
The American Society of Anesthesiologists (ASA), along with ASA Pain Committee Chair, Asokumar Buvanendran, M.D., were acknowledged by the Chief Medical Officer for the Office of the Assistant Secretary for Health in the Department of Health and Human Services (HHS) for demonstrating early support of the HHS Pain Management Best Practices Inter-Agency Task Force and for providing input on best practice recommendations for acute and chronic pain. Congratulations to Dr. Buvanendran!
Image
David M. Rothenberg, MD, FCCM, Receives the Distinguished Service Award for " Outstanding Contributions to the Advancement of Anesthesiology in Illinois from the Illinois Society of Anesthesiologists
Asokumar Buvanandran, MD, Appointed President of American Society of Regional Anesthesia and Pain Medicine
Image
Originally founded in 1923, ASRA was reborn in 1975 and is the largest subspecialty medical society in Anesthesiology. With approximately 4,500 members, the society has rich international distribution and rising attendance at annual meetings and scientific presentations. Dr. Buvanendran's ASRA presidency will last through April 2019 and include hosting the World Congress of Regional Anesthesia and Pain Medicine, an event not scheduled to occur in the United States for another 24 years and expected to attract more than 3,000 delegates.
-
Resident News
American Society of Anesthesiologists
October 10-14, 2025 | San Antonio, TX
Thank you to the following Rush residents that presented:
Christine Chin, DO and Graham Lubinsky, MD, FASA: RE-expansion Pulmonary Edema after Chest Tube during Orthotopic Liver Transplantation.
Paul Eapen, MD and Shuchi Jain, DO: When Hospice Isn't the End: A Case Study in Prognostic Reevaluation and Shared Decision-Making.
Ashleigh Gore, DO and Graham Lubinsky, MD, FASA : Catecholamine Surge During Adrenal Manipulation.
Young Jae Kim, MD and Denis Snegovskikh, MD : Airway Challenges in a Young Female with Teratoma.
Tirth S. Patel, DO, Shuchi Jain, DO and Sarah Cocoma, MD : No Blood? No Problem!-Navigating Critical Anemia in a Jehovah's Witness Patient.
Michael Schmitz, MD and Michael Dorsi, MD: Challenges in Ventilatory Management Cardiogenic Oscillations Leading to Autotriggering.
Andy Wu, MD and Graham Lubinsky, MD, FASA: Management of TVA for Liver Transplant in the Setting of Massive Blood Loss.
Resident, Richard Wang, featured in US News & World Report
Oct 15, 2025
Read the Article by clicking link below
Fentanyl-Linked Overdose Deaths Among Seniors Soar 9,000% in Eight Years
Society for Obstetric Anesthesia and Perinatology
April 31-May 4, 2025 | Portland, OR
Thank you to the following Rush resident that presented:
Sunny Patel, MD and Edelberto Perez, MD: Platelet Storage Pool Disorder in a Paturient
Midwest Anesthesia Regional Conference
April 25-27, 2025 | Indianapolis, IN
Hosted by: Indiana University, University of Louisville, and University of Toledo
Congratulations to our Anesthesiology residents who earned 5 awards!
Ryan Cournoyer, MD and Robert McCarthy, PharmD: TEA vs ESPB *3rd Place in Basic Science
Connor Ford, MD and Graham Lubinsky, MD, FASA: OLT with Known Effusion. Inability to Ventilate Post Induction. Emergent Chest Tube. Re-Expansion Pulmonary Edema.*3rd Place in CVT
Young Jae Kim, MD and Tolga Suvar, MD: Kearns Sayre Syndrome. *2nd Place in Patient Safety
Alexa Roy, MD and Deepali Garg, MD: Seizure, Case Series. *1st Place in Neuroscience
Austin Tisdell, DO and Lindsay Nowak, MD: Incidental Chronic Large Pericardial Effusion. *1st Place in General
Congratulations to all our residents for their outstanding performance including:
- Jake Abramowicz, DO
- Joshua Chiang, MD
- Christine Chin, DO
- Anthony Delehanty, MD
- Alexander Doudnikoff, MD
- Tom George, MD
- Ashleigh Gore, DO
- Austin Hake, MD
- Ryan Johnson, DO
- Samuel Johnson, DO
- Saagar Menon, MD
- Kailash Panchapakesan, MD
- Nandeeta Patel, DO
- Priyanka Patel, MD
- Andrew Pund, DO
- Joe Puthumana, MD
- Michael Schmitz, MD
- Aashaka Shah, MD
- Roman Solecki, MD
- Rafael Victorio, Jr, DO
Also, congratulations to our Rush Medical College MD candidate, Zoe Bilello for earning 2nd place in Basic Science. Outstanding performance at MARC 2025!
Society of Cardiovascular Anesthesiologists
April 24-30, 2025 | Montreal, Canada
Thank you to the following Rush residents that presented:
Paul Eapen, MD and Alaeddin Tarhuni, MD: Management of Intracardiac Hematoma After Triple-vessel CABG
Antonia Lin, MD and Arvind Rajagopal, MD: Incidentally Discovered Patent Ductus Arteriosus in Patient Receiving Aortic Valve Replacement and Mitral Valve Repair
Ashfique Nazib, DO and Arvind Rajagopal, MD: Incidental Finding of Aortic Valve Mass via Transesophageal Echocardiogram During Elective Coronary Artery Bypass Graft
Prayag Pershad, MD and Arvind Rajagopal, MD: The Utility of a Bronchial Blocker for Lung Isolation in Setting of Unanticipated Tracheal Injury
Society of Pediatric Anesthesia
March 28-30-22, 2025 | Orlando, FL
Thank you to the following Rush resident that presented:
Ankita Kadarmandalgi, DO and Alina Lazar, MD: Spinal Anesthesia for Laparoscopic Gastrostomy Tube Placement in an Infant with Epidermolysis Bullosa
American Society of Anesthesiologists
October 18-22, 2024 | Philadelphia, PA
Thank you to the following Rush residents that presented:
Antonia Lin, MD and Graham Lubinsky, MD, FASA: Anaphylaxis to Anti-thymocyte Globulin in a Renal Transplant.
Michael Nemsick, MD and Sandeep Amin, MD: Intrathecal Pump Failure Secondary to a Proximal Versus the More Common Distal Catheter Obstruction.
Nandeeta Patel, DO: Preoperative Assessment and Optimization of a Complex Patient with Renal Mass with IVC Thrombus with h/o Alcoholic Cirrhosis and Severe Hypothyroidism (TSH 373) for Excision of Renal Mass and IVC Thrombus.
Justin Shang, DO and Deepali Garg, MD: Considerations for a Patient with Isovaleric Acid CoA Dehydrogenase Deficiency Undergoing Craniectomy.
Andy Wu, MD and Arvind Rajagopal, MD: Intraoperative Management of Patient with Alkaptonuric Ochronosis Undergoing Coronary Artery Bypass Graft and Reoperative Aortic Valve Replacement: A Case Report.
Society for Obstetric Anesthesia and Perinatology
May 2-5, 2024 | Denver, CO
The following Rush residents presented:
Jared Keele, DO and Edelberto Perez, MD: May-Hegglin Anomaly in Pregnancy: Cesarean Section with Severe Thrombocytopenia
Aaran Varatharajan, MD and Edelberto Perez, MD: Hypofibrinogenemia in Pregnancy: AFLP vs HLH
Society of Cardiovascular Anesthesiologists
April 26-30, 2024 | Toronto, Canada
The following Rush resident presented:
Annie Yao, MD and Arvind Rajagopal, MD: Anesthetic Considerations for Neuromonitoring During a Thoracotomy
Midwest Anesthesia Regional Conference
April 5-7, 2024 | Omaha, NE
Hosted by: University of Nebraska, University of Missouri (Kansas City), University of Kansas (Kansas City) and University of Kansas (Wichita)
Congratulations to our Anesthesiology residents who earned 4 awards!
Antonia Lin, MD and Vaskar Das, PhD: EVALUATION OF THE ANALGESIC ACTIVITY OF CO-ADMINISTRATION OF
(2R,6R)-HYDROXYNORKETAMINE WITH MELOXICAM IN MURINE MODEL OF
LOW BACK PAIN. *3rd Place in Basic ScienceSunny Patel, MD and Vaskar Das, PhD: EFFECT OF (2R,6R)-HYDROXYNORKETAMINE ON C-FOS EXPRESSION IN
MURINE MODEL OF BACK PAIN.*1st Place in Basic ScienceDylan Shives, DO and Graham Lubinsky, MD, FASA: VENO-VENOUS ECMO IN A 35-WEEK PREGNANT PATIENT REQUIRING
TRACHEAL DILATION. *2nd Place in AirwayJihee Yoon, MD and Behnoosh Shayegan, MD: IMPORTANCE OF OPTIMIZATION IN DIFFICULT AIRWAY MANAGEMENT. *3rd Place in Airway
Congratulations to all our residents for their outstanding performance including:
- Thomas Beres, MD
- James Burke, MD
- Paul Eapen, MD
- Emma Hall, DO
- Ankita Kadarmandalgi, DO
- Ryan Knox, MD
- Brady McCaffrey, DO
- Michael Nemsick, MD
- Tirth Patel, DO
- Prayag Pershad, MD
- John Popovich, DO
- Zachary Radwanski, DO
- Katherine Thompson, DO
- Brendan Van Iten, DO
- Philip Vazquez, MD
- Andy Wu, MD
North American Neuromodulation Society
January 18-21, 2024 | Las Vegas, NV
Thank you to the following Rush resident that presented:
Rushad Marfatia, MD
ASRA Pain Medicine Meeting
November 10-11, 2023 | New Orleans, LA
Thank you to the following Rush residents that presented:
Stephen Music, DO
Sanam Solanki, MD
Michael Hunter Webb, MD
Zachary Radwanski, DO
American Society of Anesthesiologists
October 18-22, 2023 | San Francisco, CA
Thank you to the following Rush residents that presented:
Shyam Desai, MD
Ethan Parnass, MD
Justin Shang, DO

American Society of Pain and Neuroscience
July 13-16, 2023 | Miami Beach, FL
The following Rush resident presented:
Shyam Desai, MD, Christopher Massey, MD and Sandeep Amin, MD: Escheria coli Backterial Meningitis after Intrathecal Pump Implantation.
Society of Cardiovascular Anesthesiologists
May 6-9, 2023 | Portland, OR
The following Rush resident presented:
Bishir Clayton, MD and Arvind Rajagopal, MD: Undiagnosed Antiphospholipid Syndrome in a Patient Preparing To Undergo Open Heart Surgery for Mitral Valve Regurgitation
Society for Obstetric Anesthesia and Perinatology
May 3-7, 2023 | New Orleans, LA
The following Rush residents presented:
Justin Shang, DO and Michael Holland, MD: Anesthetic Considerations for a Parturient with Subglottic Stenosis and Multiple Sclerosis
Daniel Webster, MD and Alisha Bhatia, MD: An Uncommon Initial Presentation of Amniotic Fluid Embolism
Midwest Anesthesia Regional Conference
April 14-16, 2023 | Milwaukee, WI
Hosted by: Medical College of Wisconsin & University of Wisconsin Hospital & Clinics
Congratulations to our Anesthesiology residents who earned 5 awards!
Bishir Clayton, MD and Neal Mehta, MD: Analgesic and Opioid Sparing Effect of Postoperative Bilateral Erector Spinae Plane Infusions in Adolescent Scoliosis Surgery. *3rd Place in Pediatrics (Regional)
Jared Keele, DO and Vaskar Das, PhD: Gender Dependent Allodynic Responses to Disc Puncture in a Murine Model of Low Back Pain. *3rd Place in Basic Science
Jungmin On, DO and Vaskar Das, PhD: Effect of a-Amino-3-Hydroxy-5-Methyl-4-Isoxazolepropionic Acid Receptor (AMPA) Dependent Glutamate A1 and Glutamate A2 Activation on Hippocampal Pain Pathways in a Murine Model of Complex Regional Pain Syndrome.*1st Place in Basic Science
Yeon Park, MD and Robert McCarthy, PharmD: Evaluating Missingness in an Obstetric Anesthesia Study Utilizing Electronic Survey Data Capture: Implication on Study Bias. *1st Place in OB
Aaran Varatharajan, MD and Timothy Lubenow, MD: Successful Treatment of Refractory Neuropathic Pain Following Axillary Dissection and Lipoma Resection Using Cervical and Thoracic Dorsal Root Ganglion Stimulation. *1st Place in Pain
Congratulations to all our residents for their outstanding performance including:
- Shyam Desai, MD
- Esther Galant, MD
- Brett Geever, MD
- Mateusz Graca, MD
- Daniel Hamburger, MD
- Ryan Hoium, DO
- Young Soo Hong, MD
- Jennifer Huh, MD
- Russell Igarashi, DO
- Andrew Keeney, MD
- Ian Kolata, MD
- Rushad Marfatia, DO
- Elizabeth Morin, MD
- Christopher Reglen, MD
- Justin Shang, DO
- Sanam Solanki, MD
- Armaan Trivedi, DO
- Michael Hunter Webb, MD
- Daniel Webster, MD
- Annie Yao, DO
Congratulations to our Rush Medical College MD candidate, Autumn Moore for her outstanding performance at MARC 2023!
Society of Critical Care Anesthesiologists
April 14-15, 2023 | Denver, CO
The following Rush resident presented:
Jessica Richelieu, MD and Alisha Bhatia, MD: Perioperative management of abdominal compartment syndrome.
American Academy of Pain Medicine
March 23-26, 2023 | Ft. Lauderdale, FL
The following Rush residents presented:
Ethan Parnass, MD, Christopher Massey, MD and Matthew Jaycox, MD: Complex Regional Pain Syndrome After Influenza Immunization.
Aaran Varatharajan, MD, and Matthew Jaycox, MD: Case Report: Acute Guillain-Barre Syndrome After SI Joint Fusion.
Image
North American Neuromodulation Society
January 12-15, 2023 | Las Vegas, NV
The following Rush resident presented:
Mateusz Graca, MD, Haley Wardrip, MD and Timothy Lubenow, MD: Cervical and High-Thoracic Dorsal Root Ganglion Stimulation for Complex Regional Pain Syndrome of the Upper Extremities
Image
Regional Anesthesiology and Acute Pain Meeting
November 17-19, 2022 | Orlando, FL
The following Rush resident presented:
Stephen Music, DO, Nathan Wick, DO and Tolga Suvar, MD: Cervical & High Thoracic Spinal Cord Stimulation to Treat Refractory Chronic Neck & Low Back Pain in Failed Back Surgery Syndrome
Image
American Society of Anesthesiologists
October 21-25, 2022 | New Orleans, LA
Thank you to all the Rush residents that presented:
Ali Bazzi, DO
Deepali Garg, MD
Sara Izzo, DO
Stephen Music, DO
Image
Midwest Anesthesia Regional Conference
April 29-May 1, 2022 | St. Louis, MO
Hosted by University of Missouri-Columbia, St. Louis University, Washington University-St. Louis, University of Iowa
Congratulations to our Anesthesiology residents who earned 8 awards!
Sara Boldt, DO and Margaret Griesemer, DO: Analgesic Effectiveness and Opioid Sparring Properties of the Erector Spinae Plane Block, Thoracic Epidural and IV Patient Controlled Analgesia Following Esophagectomy: A Retrospective Comparison *1st Place in Regional
Nathaniel Donnell, MD and Sandeep Amin, MD: Delayed Allergic Reaction after Spinal Cord Stimulator Implantation *2nd Place in Pain Medicine
Russell Igarashi, DO and Vaskar Das, PhD: Effect of opioid and AMPA Antagonists on (2R,6R)-HNK (Hydroxynorketamine) Anti-hyperalgesic Activity in a Murine Model of Low Back Pain *1st Place in Basic Science
Yeon Park, MD and Michael Holland, MD: The Association of Pain Catastrophizing with Labor Pain and Analgesic Use *1st Place in OB Anesthesia
Alex Sadauskas, MD and Asokumar Buvanendran, MD: Clinical characteristics and surgical factors associated with postoperative pain trajectories over the first 28 days following surgery. *3rd Place in Pain Medicine
Theodore Stewart-Hester, DO and Neal Mehta, MD: Novel approach to integrating erector spinae plane block catheters in multimodal anesthesia for scoliosis surgery *2nd Place in Regional Anesthesia
Varun Takanti, MD and Vaskar Das, PhD: Cartilage Specific Deletion of PKCδ in Osterix Increases Joint Pain in Mouse Osteoarthritis Model *3rd Place in Basic Science
Ellen Zhou, MD and Christopher O’Connor, MD: Perils of Lidocaine on Induction *3rd Place in Patient Safety
Congratulations to our Rush medical student who earned an award!
Sofia Armengol, MD and Edmund Mangahas, MD: Etomidate Infusion for the Management of Cushing’s Syndrome *1st Place in General Anesthesia
Congratulations to all our residents for their outstanding performance including:
- Kimberly Allen, MD
- John Baddour, DO
- Arya Bekhradi, MD
- Mark Blazel, DO
- Bishir Clayton, MD
- Shyam Desai, MD
- Hemanth Garapati, MD
- Mateusz Graca, MD
- Daniel Hamburger, MD
- Collin Hubler, MD
- Theodore Jeske, DO
- Andrew Keeney, DO
- Jared Konner, DO
- David Lee, DO
- Michael McGinnis, MD
- Stephen Music, DO
- Ethan Parnass, MD
- Jessica Richelieu, MD
- Jayne Slocum, MD
- Timothy Swiatkowski, MD
- Aaran Varatharajan, MD
- Nathan Wick, DO
- Daniel Webster, MD
Image
March 18-21, 2022| Virtual
The following Rush resident presented:
Yogesh Taheem, MD and Amod Sawardekar, MD: Institutional Experience with Regional Anesthesia in Pediatric Renal Transplantation with Comparison to No Regional Anesthesia: A Retrospective Review of 68 Patients
Image
March 18, 2022| Virtual
The following Rush resident presented:
Tara Mojtahed, MD and Lisa Solomon, DO: Perioperative management of abdominal compartment syndrome
Image
Regional Anesthesiology and Acute Pain Meeting
November 18-20, 2021 | San Francisco, CA
The following Rush resident presented:
Nathan Wick, DO and Tolga Suvar, MD: An Algorithmic Approach to Diagnosing Intrathecal Drug Delivery Device Complications: A Case Report
Image
American Society of Anesthesiologists
October 8-12, 2021 | San Diego, CA
Thank you to the following Rush residents that presented:
Mateusz Graca, MD
Sara Izzo, DO
Tara Mojtahed, MD
Michael Petravick, MD
Alexi Pollet, DO
Haley Wardrip, MD
Tony Zhang, MD
Image
Midwest Anesthesia Regional Conference
April 16-18, 2021 | Virtual
Hosted by Rush University Medical Center and Cook County Health
Congratulations to our Anesthesiology residents who earned 11 awards!
The following Rush residents presented:
Nkoli Akaolisa, MD and Alaeddin Tarhuni, MD: Biventricular Support in a Patient with COVID Associated Myocarditis *1st Place in Cardiovascular
Deepali Garg, MD and Alisha Bhatia, MD: Sedation Compared to General Anesthesia During Mechanical Thrombectomy: A Retrospective Analysis of Outcomes in Subjects with Matched NIH Stroke Scores and Age at Presentation *3rd Place in Neuroanesthesia
Keena Kohl, MD and Vaskar Das, PhD: Effect of a-Amino-3-Hydroxy-5-Methyl-4-Isoxazolepropionic Acid Receptor (AMPA) Dependent Glutamate A1 and Glutamate A2 Activation on Hippocampal Pain Pathways Following Hind-paw Incision in Mice *1st Place in Pain Medicine
Michael McGinnis, MD and Vaskar Das, PhD: Time Course of Glial Cell Activation in a Murine Model of Osteoarthritis Pain *2nd Place in Basic Science
Yabtsega Moges, MD and Arvind Rajagopal, MD: Delirium in Elderly Patients Undergoing Outpatient Surgical Procedures: A Randomized Clinical Trial of an Avoid Delirium Protocol *1st Place Award in Ambulatory
Michael Petravick, MD and Shruti Bassi, MD: Endoscopic Resection of a Juvenile Nasopharyngeal Angiofibroma in a 14 Year Old Male with Multiple Bleeding Disorders and Recent SARS COV-2 *1st Place in Pediatrics
Michael Petravick, MD and Alisha Bhatia, MD: Sudden Onset Rigidity, Apnea, Tachycardia, and Hypertension in a Patient Undergoing Awake Craniotomy for Anaplastic Astrocytoma *3rd Place in Neuroanesthesia
John Ward, MD and Vaskar Das, PhD: Effect of Opioid and AMPA Antagonists on (2R, 6R)-HNK (Hydroxynorketamine) Anti-hyperalgesic Activity *2nd Place in Pain Medicine
Nathan Wick, DO and Vaskar Das, PhD: Peripheral Adenosine Mono-phosphate Activated Kinsas Alpha as a Novel Analgesic Target for Chronic Low Back Pain *2nd Place Award in Pain Medicine
Nathan Wick, DO and Tolga Suvar, MD: Clinical Presentation and Diagnosis of Fractured Intrathecal Catheter *3rd Place Award in Pain Medicine
Tony Zhang, MD and Alisha Bhatia, MD: Intraoperative Bilateral Lower Extremity Paralysis During Surgical Correction of Progressive Adolescent Idiopathic Scoliosis *3rd Place in Neuroanesthesia
Congratulations to all our residents for their outstanding performance including:
- Ali Bazzi, DO
- Sara Boldt, DO
- Shyam Desai, MD
- Mateusz Graca, MD
- Clinton Gunn, MD
- Shakeem Iyamah, MD
- Jared Konner, DO
- Sandra Miskiewicz, DO
- Norman LaCombe, MD
- Tara Mojtahed, MD
- Maxwell Muench, DO
- Taylor Pierce, MD
- Alexander Ryder, DO
- Luis Sanguino, MD
- Michael Sparks, MD
- Timothy Swiatkowski, MD
- Yogesh Taheem, MD
- Haley Wardrip, MD
Image
American Society of Anesthesiologists
October 19-23, 2019 | Orlando, Florida
Thank you to all the Rush residents that presented
American Society of Anesthesiologists
Image
The Society of Obstetric Anesthesia and Perinatology
51st Annual Meeting
May 1- 5, 2019 | Phoenix, Arizona
The following Rush residents presented:
John Gburek, MD and Laurie Mark, MD: Obstetrical Considerations and Management of Labor and Delivery of a G1P0 Woman with a History of Multiple Liver Transplants.
Anna Sobilo, MD and Michael Holland, MD: Cesarean Section in a Parturient with Congenital Cardiomyopathy, Complicated by Ventricular Bigeminy.
Society for Obstetric Anesthesia and Perinatology
Image
Society of Critical Care Anesthesiologists 32nd Annual Meeting and Critical Care Update
May 17, 2019| Montreal, Quebec
The following Rush residents presented:
Angella Koncarevic, MD and Alisha Bhatia, MD: The Role of Plasma Exchange in the Treatment of West Nile Virus Neuroinvasive Disease.
Jessica Kruse, MD and Laurie Mark, MD: A Difficult Airway in the ICU: Complicated by a Bronchoesophageal Fistula.
Society of Critical Care Anesthesiologists
ImageInternational Anesthesia Research Society Annual Meeting and International Science Symposium
May 18-21, 2019 | Montreal, Quebec
The following Rush residents presented:
Daryl Kerr, MD and Mary Rhee, MD: Anesthetic Management of Metastatic Chondrosarcoma to the Right Atrium in the setting of a Right-to-Left Intracardiac Shunt.
International Anesthesia Research Society
ImageSociety of Cardiovascular Anesthesiologists Thoracic Symposium
May 17, 2019 | Chicago, IL
The following Rush residents presented:
Yeona Chun, MD and Arvind Rajagopal, MD: Serratus Anterior Plane Block for Staged Thoracic Outlet Decompression in Paget-Schroetter Syndrome.
Jordan Schell, MD and Kristine Pearson-Chauhan, DO: Re-expansion Pulmonary Edema.
Lida Shaygan, MD and Pete Pelletier, MD: Postoperative Serratus Anterior Plane Continuous Catheter as an Analgesic Rescue Technique, after a Failed Thoracic Epidural, for an Ivor Lewis Esophagectomy with Laparotomy and Right Sided Thoracotomy.
Society of Cardiovascular Anesthesiology
ImageSociety of Cardiovascular Anesthesiologists 41st Annual Meeting
May 18-21, 2019 | Chicago, IL
The following Rush residents presented:
Lawrence Kopsick, MD and Kristine Pearson-Chauhan, DO: The Anesthetic Considerations of Video-Assisted Thoracoscopy Surgery in a Patient with Kartagener’s Syndrome.
Jonathan Schirripa, MD and Brian Birmingham, MD: Transhepatic Access for Left Atrial Appendage Closure Device Complicated by Subcapsular Hematoma.
Avanthi Tudor, MD and Kristine Pearson-Chauhan, MD: Management of Ventricular Septal Defect Post Bacterial Endocarditis.
Society of Cardiovascular Anesthesiology
ImageRegional Anesthesiology and Acute Pain Meeting
April 11-13, 2019 | Las Vegas, NV
The following Rush residents presented:
Bryce Austell, MD and Pete Pelletier, MD: Bilateral Erector Spinae Catheters for Analgesia in Sternectomy.
John Ha, DO, Arjun Ramesh, MD, Robert McCarthy, PhD, and Neil Mehta, MD: Factors Associated with Failed Supraclavicular Brachial Plexus Nerve Block in Upper Extremity Surgery.
Inderbir Johal, MD: Total Knee Arthroplasty Solely Utilizing Peripheral Nerve Blockade and Sedation.
Alexandra Lelchuk, MD: Determination of Clinically Important Cut-off Values of Pain Catastrophizing for Predicting Increased Postoperative Pain Following Total Knee Arthroplasty.
Raj Patel, MD and Alisha Bhatia, MD: Neuraxial Anesthesia for Below Knee Amputation in the Setting of Gangrene and Untreated 3-vessel Coronary Artery.
Arjun Ramesh, MD, Nathaniel Froikin, BS, Yabtsega Moges, MD, and Asokumar Buvanendran, MD: Transversus Abdominis Plane Block Improves Outcomes and Reduces Discharge Time in an Enhanced Recovery from Anesthesia and Surgery Protocol in Patients Undergoing Laparoscopic Bariatric Surgery.
Salman Sagarwala, MD and Aris Austin, MD: Erector Spinae Plane Catheter for Postoperative Analgesia in a Patient Undergoing Resection of Pancoast Tumor.
Hemanth Sirandas, MD and Neal Mehta, MD: Gastric Content Assessment Utilizing Point-Of-Care Ultrasound (POCUS) in a Patient with Questionable NPO Status.
American Society of Regional Anesthesia and Pain Medicine
ImageAnnual Midwest Anesthesia Regional Conference
April 12-14, 2019 | Detroit, MI
Hosted by Beaumont, Detroit Medical Center, Henry Ford Health Systems, McLaren Greater Lansing, University of Michigan, and Wayne State University
Congratulations to our Anesthesiology residents who earned a total of 16 awards!
The following Rush residents presented:
Kolawole Akinduro, DO and Kristine Pearson-Chauhan, DO: A Rare Case of Endogenous Endopthalmitis in a Pregnant Woman with Pyelonephritis.
Sherry Bhowra, MD and Neal Mehta, MD: Gastric Content Assessment Utilizing Point-of-Care Ultrasound in a Patient with Questionable NPO Status.
Patrick Binetti, MD and Behnoosh Shayegan, MD: Airway Management of a Fetus with a Craniofacial Abnormality During Operation on Placental Support (OOPS) Procedure.
*2nd Place in Pediatrics
Yulong Chen, MD and Alexander Froyshteter, MD: Dusky Blue Skin Discoloration after Isosulfan Blue Injection.
Yeona Chun, MD and Alexander Froyshteter, MD: Perioperative Glucose Monitoring Utilizing an Implanted Monitoring System in a Pediatric Patient.
* 1st Place Award in Pediatrics
Yuriy Davydov, MD and Kristine Pearson-Chauhan, DO: Acute Hypotensive Transfusion Reaction.
Mardia Elfakhery, MD and Brian Birmingham, MD: Transhepatic Access for Left Atrial Appendage Closure Device Complicated by Subcapsular Hematoma.
Mukund Gande, MD and Nitesh Mody, DO: Extracorporeal Membrane Oxygenation in a Patient with Acute Respiratory Distress Syndrome and Disseminated Histoplasmosis.
*1st Place Award in Critical Care
John Gburek, MD and Michael Holland, MD: Obstetrical Considerations and Management of Labor and Delivery of a G1P0 Woman with a History of Multiple Liver Transplants.
Salvin Jacob, MD and Jeffrey Kroin, PhD: The Ketamine Metabolite (2R, 6R)-HNK Reduces Allodynia in Neuropathic Pain Mice.
*2nd Place Winner - Association of Midwest Academic Anesthesia Chair Award for Basic Poster Presentations
Drew Jensen, MD and Alisha Bhatia, MD: Airway Management in a Patient with Cervical Neck Trauma and Fresh Tracheostomy Requiring Lung Isolation for Right-sided VATS, Wedge Resection, and TALC Pleurodesis.
Lawrence Kopsick, MD and Kristine Pearson-Chauhan, DO: The Anesthetic Considerations of Video-assisted Thoracoscopy Surgery in a Patient with Kartagener’s Syndrome.
Jessica Kruse, MD and Asokumar Buvanendran, MD: Tap Block Improves Outcomes and Reduces Discharge Time in an Enhanced Recovery from Anesthesia and Surgery Protocol in Patients Undergoing Laparoscopic Bariatric Surgery.
* 2nd Place in Regional
Ryan Kuta, DO and Kristine Pearson-Chauhan, DO: Peripheral Nerve Blockade as the Primary Anesthetic for Total Knee Arthroplasty.
Norman LaCombe, MD and Jeffrey Kroin, Ph.D.: Early Treatment with Metformin Reduces Pain in a Mice Model of Complex Regional Pain Syndrome (CRPS).
*3rd Place Winner - Association of Midwest Academic Anesthesia Chair Award for Basic Poster Presentations
Nabila Malik, MD and Asokumar Buvanendran, MD: Factors Associated with Failed Supraclavicular Brachial Plexus Nerve Block in Upper Extremity Surgery.
Shefali Mandhle, MD and Arvind Rajagopal, MD: Serratus Anterior Plane Block for Staged Thoracic Outlet Decompression in Paget-Schroetter Syndrome.
*3rd Place in Regional
Teuta Marsic, MD and Anna Dziamski, MD. Management of Intra-operative Anaphylaxis of Unknown Origin in a Female Undergoing Breast Reconstruction Surgery.
Teuta Marsic, MD and Neal Mehta, MD: Bilateral Erector Spinae Plane Continuous Catheter as analgesic Technique for Sternectomy with Chest Wall Chondrosarcoma Resection and Reconstruction.
*3rd Place in Regional
Pranusha Naidu, MD and Sandeep Amin, MD: Diagnosis of a Severed Intrathecal Pump Catheter using Ultrasound and Fluoroscopy.
Rodd Rezvani, MD and Jeffrey Kroin, PhD: Bone Biomarker Upregulation in a Tibia Fracture Model of Complex Regional Pain Syndrome in Mice.
Rodd Rezvani, MD and Alexander Froyshteter, MD: A Difficult Anatomical and Physiological Airway Outside the Operating Room.
Jordan Schell, MD and Kristine Pearson-Chauhan, DO. Re-expansion Pulmonary Edema.
* 3rd Place In Cardiovascular
Phillip Standen, DO and Alisha Bhatia, MD: Right-sided Paratracheal Mass: A Case of Progressive Dyspnea and Hypoxemia Refractory to Intubation.
*3rd Place in Airway
Mark Anthony Sy, MD and Arvind Rajagopal, MD: Perioperative Management of Jehovah’s Witnesses.
Morgan Ulloa, MD and Alexander Froyshteter, MD: Anesthetic Management of Pediatric Patients with Niemann-Pick Disease Type C for Intrathecal 2-Hydroxypropyl-β-Cyclodextrin Injection.
*1st place Honors
Morgan Ulloa, MD and Alisha Bhatia, MD: Clinical Validation of StimpodTM Acceleromyography and Electromyography.
* 1st Place Honors
Keziah Vargas, MD and Alisha Bhatia, MD: Laryngospasm and Difficult Airway in a Foreign Body Aspiration Retrieval.
Zerghona Wadood, MD and Alisha Bhatia, MD: West Nile Virus Neuroinvasive Disease.
*3rd Place in Critical Care
Jaclyn Yeung, DO and Laurie Mark, MD: A Case of Epiglottitis in an Immunocompromised Adult
*3rd Place in Airway
Rena Zheng, MD and Asokumar Buvanendran, MD: Determination of Clinically Important Cut-off Values of Pain Catastrophizing for Predicting Increased Postoperative Pain following Total Knee Arthroplasty.
Congratulations to all our residents for their outstanding performance including:
- Kola Akinduro, MD
- Sherry Bhowra, MD
- Yulong Chen, MD
- Yuriy Davydov, MD
- Mardia Elfakhery, MD
- John Gburek, MD
- Drew Jensen, MD
- Lawrence Kopsick, MD
- Ryan Kuta, MD
- Pranusha Naidu, MD
- Rodd Rezvani, MD
- Mark Sy, MD
- Keziah Vargas, MD
- Nabila Malik, MD
- Rena Zheng, MD
Association of Midwest Academic Anesthesia Chairs - Sponsor of the MARC Conference
ImageSociety for Pediatric Anesthesiology
March 15-17, 2019| Houston, TX
The following Rush residents presented:
Jenny Chan, MD and Alexander Froyshteter, MD: Skin Lesions and Airway Obstruction: Be Mindful of Mediastinal Masses.
Yeona Chun, MD and Alexander Froyshteter, MD: Perioperative glucose monitoring utilizing an implanted monitoring system in a pediatric patient.
Leili Khorassani, MD and Behnoosh Shayegan, MD: The Operation on Placental Support (OOPS) Procedure for Airway Management of a Fetus with a Craniofacial Abnormality.
Society for Pediatric Anesthesiology
ImagePostgraduate Assembly in Anesthesiology
December 7-11, 2018| New York, NY
The following Rush residents presented:
Daryl Kerr, MD and Jesse H. Marymont, MD: Intraoperative Use of Impella Device for ON-PUMP Coronary Artery Bypass Graft.
Postgraduate Assembly in Anesthesiology
ImageRegional Anesthesiology and Acute Pain Meeting
November 15-17, 2018| San Antonio, TX
The following Rush residents presented:
Mitchell Bosman, MD and Sandeep Amin, MD: Use of Dorsal Root Ganglion Stimulation in Post- Thoracotomy Pain Syndrome after Failed Spinal Cord Stimulation.
Ryan Kuta, DO and Timothy Lubenow, MD: Neuromodulation in a Patient with Adult Tethered Spinal Cord Syndrome.
Shefali Mandhle, MD and Timothy Lubenow, MD: The Use of Dorsal Root Ganglion Stimulation for Back Pain Secondary to Failed Back Surgery Syndrome.
Raj Patel, MD and Timothy Lubenow, MD: Dorsal Root Ganglion Stimulation in the Treatment of Chronic Osteoarthritis Knee Pain.
Salman Sagarwala, MD and Timothy Lubenow, MD: DRG Stimulation in a Patient with CRPS Following Back Surgery.
American Society of Regional Anesthesia and Pain Medicine
Image
American Society of Anesthesiologists
San Francisco, CA | October 13-17,2018
13 Faculty Research Studies Presented by:
Asokumar Buvanendran, MD
Timothy R. Lubenow, MD
Robert J. McCarthy, PharmD
Jeffrey S. Kroin, PhD
Mario Moric, MS
Vaskar Das, PhD
10 Resident Case Reports presented by:
Jenny Chan, DO
Salman Sargawala, MD
Hemanth Sirandas, MD
Alan F. Molina, MD
Lida Shaygan, DO
Faculty Mentors:
Arvind Rajagopal, MD
Kristine Pearson-Chauhan, DO
Behnoosh Shayegan, MD
Anna Sobilo, MD
Phillip Standen, DO
Hung Tran, MD
Jaclyn Yeung, DO
Avanthi Tudor, MD
Laurie Mark, MD
Neal Mehta, MD
Asokumar Buvanendran, MD
Congratulations to Vaskar Das, Ph.D. who received the top award in the Young Investigator Basic Science ( Cancer and Chronic Pain Category) for his study: Degenerative Disc Pain in Mouse Model.
American Society of Anesthesiologists
ImageMidwest Anesthesia Residents Conference
Cincinnati, Ohio | April 13-15, 2018
Dr. Raj Patel, Dr. Jeffrey S. Kroin, Dr. Vskar Das, PhD, and Dr. Asokumar Buvanendran: Can Biphosphonate Drugs Prevent Pain a Mouse CRPS Model?
* 1st Place Award in the Basic Science Category
Dr. Morgan Ulloa, Dr. Jefferey S. Kroin, Dr. Vskar Das, and Dr. Asokumar Buvanendran: Changes in Pain Mediators in Mouse Dorsal Root ganglion after Bone Fracture
* 2nd Place Award in the Basic Science Category
Dr. Michael Warren, Dr. Asokumar Buvanendran, and Dr. Robert McCarthy: Acute Postoperative Pain in an Independent Predictor of Persistent Postsurgical Pain Following Total Knee Arthroplasty
* 1st Place Award in the Pain Studies Category
Dr. Danial Shams and Dr. Timothy Lubenow: Dorsal Root Ganglion Stimulation for Chronic Pain
* 2nd Place Award in Pain Studies Category
Dr. David Kim: Chronic Sacroiliac Joint Pain Successfully Treated with Dorsal Root Ganglion Stimulation
* 2nd Place Award in Pain Case Reports Category
Dr. Anna Sobilo and Dr. Kristine Pearson-Chauhan: Splenopneumopexy
* 2nd Place Award in the General Case Report Category
Dr. Arjun Ramesh and Patricia Perry: Anesthesthetic Management of Mirror Syndrome
* 2nd Place Award in Obstetrical Case Reports
Dr. Tran Hung and Dr. Sandeep Amin: Dorsal Root ganglion Stimulation for Chronic Pain in Charcot-Marie-Tooth Disease
* 3rd Place Award in Pain Case Reports Category
Midwest Anesthesia Residents Conference
Image
Rush Surgical Society Awards
March 21, 2018
Rush Residents Presented:
Raj Patel, MD, Vaskar Das, PhD, and Jeffrey Kroin, PhD. Can Biphosphonate Drugs Prevent Pain in Mouse CRPS Model?
* 3rd Place Winner
Image
Bryce Austell, MD and Asokumar Buvanendran, MD. Drugs Prescribed at Hospital after Surgery for Pain Control
* Finalist
Image
Resident Scores in Top 10% on ABA Basic National Exam
Congratulations to Dr. Salman Sagarwala, who scored in the top 10% on the ABA Basic National Exam. We are proud of his achievement!
ImageIrshad Siddiqui CNIM, will give a presentation at the Illinois Society of Electroneurodiagnostic Technologists Meeting
March 16, 2019 | Winfield, Illinois | DuPage Hospital
Presentation:
Irshad Siddiqui, CNIM . Monitoring the Cranial Nerves
Image
Anna Dziamski, MD wins Katalin Selmeczi, MD & Curt J. Stokes, MD Memorial Award
The award is given to the graduating resident who embodies the spirit, humanism, devotion, courage, and work ethic exemplified by Katalin Selmeczi, MD and Curt J. Stokes, MD.
Image
Kathleen L. Than, DO wins Robert D. Dripps, MD Memorial Award
The award is presented annually to the outstanding graduate resident in Anesthesiology.
