The majority of clinical training takes place at Rush University Medical Center, a tertiary care center. Other sites include Endeavor Health Skokie Hospital, Endeavor Health Glenbrook Hospital, Rush Oak Brook Surgery Center, Rush Surgicenter and Ann & Robert H. Lurie Children's Memorial Hospital.
Learn more about clinical training in each year of the program.
Clinical Base Year, CA-0
Consists of thirteen, 4-week rotations, which include the following:
- General Internal Medicine
- Cardiology
- Cardiovascular Critical Care (CICU)
- Pulmonology
- Trauma
- General Surgery
- Surgical Critical Care (SICU)
- Pain Medicine
- Emergency Medicine
- Anesthesia Preoperative Evaluation Clinic (APEC)
- Introduction to Anesthesiology
- The year concludes with two 4-week rotations in Introduction to Anesthesiology, including a comprehensive didactic series and experience in the operating room.
General Internal Medicine
Interns spend four, 4-week rotations within the Department of Internal Medicine. Residents have primary care responsibilities for patients with a vast array of medical diseases that typify a tertiary care medical center. Interns are responsible for writing orders and providing patient care. Supervising residents and attending staff organize daily and weekly teaching rounds directed towards patient care and resident education. One or two of these four-week rotations focuses on cardiac and/or medical intensive care and an elective cardiology or pulmonology.
Emergency Medicine
Interns may spend a 4-week rotation in the emergency department under the guidance of attending physicians in the Department of Emergency Medicine at Rush University Medical Center. This busy inner-city emergency department sees over 70,000 patients per year and provides the intern with the opportunity to manage patients on an acute and emergent basis. The rotation helps prepare the intern for the acute and emergent situations that frequently occur in the operating room. The call schedule is reflective of the emergency medicine rotation and usually consists of eight- to twelve-hour shifts.
General Surgery
Interns spend three 4-week rotations in the department of general surgery during their internship. They get exposed to different services within surgery during this rotation such as Transplant surgery, Trauma surgery (at Stroger Hospital at Cook Count) and also other subspecialty services such as vascular surgery or acute care surgery. Their exposure to a wide variety of surgical patients during these rotations prepares residents well for taking care of surgical patients in the operating room. Exposure to trauma at Stroger Hospital at Cook County is one of the busiest trauma units in the country and gives our trainees first hand experience in taking care of complex patients at the frontlines.
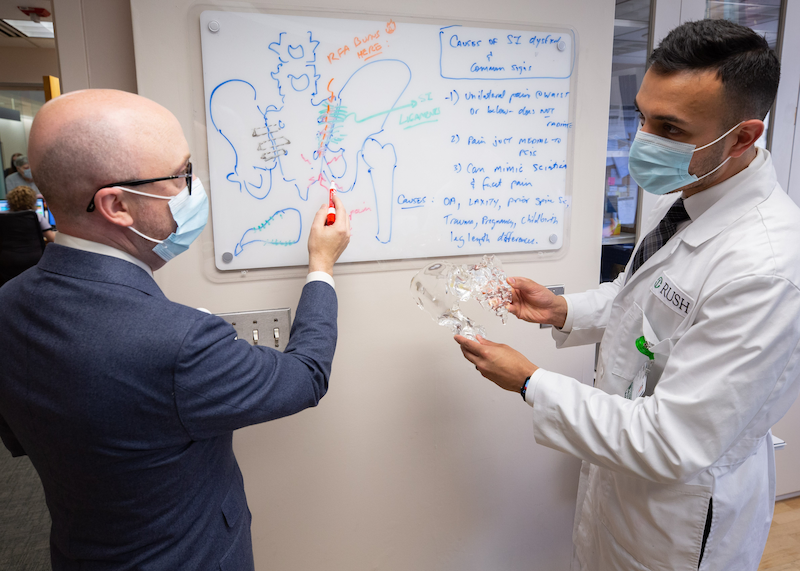
Pain Medicine
Residents spend one 4-week rotation on the pain service getting exposed to complex pain patients in the clinic setting and also interventional pain procedures in the operating room. This early exposure to one of the more sought after subspecialties in anesthesiology has solidified the desire of many of our trainees to pursue pain medicine as a fellowship after they complete their training in anesthesiology.
APEC
During the perioperative medicine rotation, residents perform pre-operative assessments in the operating room setting and also participate in the Anesthesia Preoperative Evaluation Clinic (APEC), where they serve as consultants, assessing patient risk stratification before scheduled surgical procedures under the direct supervision of an attending anesthesiologist.
SICU
This rotation is spent in the surgical ICU taking care of complex surgical patients in the postoperative period. Interns will learn how to manage hemodynamically unstable patients, patients requiring ventilatory support, manage complex airways outside the operating room in a code setting and get an understanding of other topics in critical care medicine under watchful eyes of anesthesia and surgical intensive care physicians.
Introduction to Anesthesiology
Each resident will complete two introductory months in the Department of Anesthesiology in order to gain familiarity and develop basic concepts of anesthesiology practice. Residents are assigned daily with a senior resident to either the operating room, pre-operative clinic, recovery room, regional or obstetric anesthesia and participate first hand in the management of both basic and complex cases. Emphasis is placed on performing preoperative evaluations, developing basic regional and general anesthetic management concepts, gaining intravenous access skills, and basic airway management skills. During the introductory month, residents attend an organized series of lectures and training sessions in the Rush Center for Clinical Skills and Simulation. The goal of the introductory month is to build the necessary basic knowledge and skills that will allow residents a gradual transition to the perioperative and operating room environment.
Residents do not take call during their introductory month of anesthesiology.
CA-I Year:
Consists of 13, four-week rotations that encompass the introduction to all phases of administration of general, regional and monitored anesthesia care. Resident will rotate through the following rotations:
- General Anesthesia
- Endeavor Health Skokie Hospital General Anesthesia
- Obstetrical Anesthesia
- Anesthesia Preoperative Evaluation Clinic (APEC)
- Interventional Pain Medicine
- Neurosciences Critical Care (NSICU)
- Surgical Critical Care (SICU)
- Postoperative Anesthesia Care Unit (PACU)
- Basic Regional Anesthesia
- Selective Subspecialty Rotations
General Anesthesia
Residents are assigned to care for patients undergoing routine general surgical procedures such as cholecystectomy, herniorrhaphy, appendectomy, mastectomy, as well as colon and extremity surgeries. In addition to these core procedures, residents may also be involved in surgical subspecialty cases, including plastic surgery, gynecology, ENT (ear, nose, and throat), and urology. These assignments provide broad clinical exposure and hands-on experience across both general and specialized surgical disciplines.
Basic Regional
Residents assigned to this rotation are exposed to patients undergoing orthopedic, vascular and general surgery procedures. During the basic regional rotation, residents are taught regional anesthetic techniques such as epidural, spinal, and combined spinal-epidural blocks, and the perioperative implications associated with these procedures. Residents also perform basic ultrasound guided peripheral nerve blocks during this rotation.
Perioperative Medicine / Pre-op Evaluation Clinic
During the perioperative medicine rotation, residents perform pre-operative assessments in the operating room setting and also participate in the Anesthesia Preoperative Evaluation Clinic (APEC), where they serve as consultants, assessing patient risk stratification before scheduled surgical procedures under the direct supervision of an attending anesthesiologist.
Post Anesthesia Care Unit
A two-week rotation in the post-anesthesia care unit (PACU) is a requirement for all residents and consists of assessment and management of patients in the PACU.
Pain Medicine
The Rush Pain Center is one of the Midwest's largest multidisciplinary centers, providing advanced pain management techniques to almost 12,000 patients per year. Residents evaluate and treat a wide variety of chronic and acute pain patients and participate in all aspects of patient care during the pain medicine rotation. Patients present to the Pain Center daily with problems ranging from low back pain and myofascial pain to neuropathic pain, Complex Regional Pain Syndrome (CRPS), and cancer pain.
At the Rush Pain Center, residents' responsibilities include patient evaluation, development of a treatment plan and discussion of the therapeutic options with the attending physician. When procedures are indicated, the attending physician supervises the resident in performing lumbar, thoracic and cervical epidural injections, trigger point injections, stellate ganglion blocks, intercostal nerve blocks, celiac plexus blocks, lumbar sympathetic blocks as well as a variety of less common nerve blocks. Residents gain hands-on experience in the placement of spinal cord stimulators, dorsal root ganglion stimulators, and intrathecal drug delivery systems.
In addition to the experience with chronic pain patients, there is significant exposure to management of acute pain with an anesthesiology-based acute pain team. Residents round with the acute pain team and learn how to manage pain in the postoperative period.
Obstetric Anesthesia
During the obstetric anesthesia rotation, the residents work in the Labor and Delivery (L&D) unit where there are approximately 2,500 deliveries per year, as well as other obstetric-related cases. At least 30% of the patients cared for by the maternal-fetal medicine specialists have “high-risk” pregnancies due to pregnancy-related pathologies such as preeclampsia, placental abruption, and diabetes, or due to associated comorbidities. Residents also gain experience in complex multidisciplinary anesthetics during Ex Utero Intrapartum Treatment (EXIT) and Operation On Placental Support (OOPS) procedures.
Over 80% of the patients in L&D unit utilize the obstetrical anesthesia services. Residents learn analgesic methods for routine labor, anesthetic management of cesarean section, dilation and curettage, cerclages, and tubal ligations, and become highly proficient performing lumbar epidural, combination spinal-epidural and spinal anesthetic techniques.
The residents gain expertise in fetal assessment, recognizing high-risk obstetric conditions, anticipating possible emergencies, treating maternal hemorrhage and formulating anesthetic plans that minimize maternal risk.

CA-II Year:
Consists of 13, four-week rotations that provides introduction to anesthesia subspecialties including cardiovascular/thoracic, neuro, pediatric, advanced obstetric, major orthopedic and transplant anesthesia.
A complete list of rotations include:
- Advanced General Anesthesia
- Cardiovascular/Thoracic Anesthesia
- Neuroanesthesia
- Pediatric Anesthesia
- Advanced Obstetrical Anesthesia
- Advanced Regional Anesthesia
- Surgical Critical Care (SICU)
- Neurosciences Critical Care (NSICU)
- Point-of-Care Ultrasonography (PoCUS)
- ENT/Difficult Airway
Cardiovascular / Thoracic Anesthesia (CVT)
The cardiovascular and thoracic anesthesia rotation provide exposure to a variety of cardiothoracic anesthesia cases. The spectrum of cardiac surgery cases include the CABG and valve repair/replacements, off-pump CABG and minimally invasive cardiac surgery, ascending and descending aortic aneurysm (open and endovascular repair), left ventricular assist device placement, congenital heart defect repair, transcatheter aortic valve replacement, and other interventional cardiac procedures. During this rotation, residents become skilled at the placement of arterial, central venous, and pulmonary artery catheters and also gain experience with the basic images of transesophageal echocardiography (TEE), and thoracic epidural placement, and flexible bronchoscopy. During the thoracic rotation, trainees are exposed to a wide variety of open thoracic surgical procedures, thymectomies, carinal and tracheal resections, pneumonectomies, thoracoscopic procedures, including lobectomies and segmentectomies, and esophageal surgery.
Residents have the option to rotate for four-weeks at Endeavor Health Glenbrook Hospital to obtain further cardiothoracic anesthesia training in the community setting.
Pediatric Anesthesia
The primary educational objective during the pediatric anesthesia rotation is the development of skills needed for safe delivery of anesthesia to infants and children. These skills include airway management, ventilator management and vascular access techniques. Trainees become familiar with the distinct physiologic, pharmacologic, and psychologic characteristics of infants and children, and develop preoperative, intraoperative, and postoperative assessment and anesthetic management skills.
Additional extensive training in pediatrics occurs at Ann & Robert H. Lurie Children's Memorial Hospital during the CA-2 and CA-3 year of training. Lurie Children's is ranked as the top children's hospital in Illinois according to U.S. News & World Report.

Neuroanesthesia
Rush University Medical Center is Chicago's largest center for neurosurgery, allowing residents to gain skills and knowledge of the anesthetic management of craniotomies for patients with tumors, aneurysms and AV malformations. Rush University Epilepsy Center is the referral base for epilepsy surgery and gives residents the opportunity to provide anesthetic management for these complex patients while undergoing awake craniotomies. During the neuro anesthesia rotation, residents learn neuropharmacology, neurophysiology and techniques of neurophysiologic monitoring, including processed EEG and evoked potentials.
Advanced Regional Anesthesia
This four-week clinical rotation is designed so residents expand their knowledge of the principles of regional anesthesia and gain valuable hands-on experience while performing peripheral nerve blocks for surgical patients using ultrasound technology and/or peripheral nerve stimulation techniques. Residents learn how coexisting diseases and chronic pain influence the regional anesthetic approaches and become familiar with the indications, contraindications, risks and benefits of various regional anesthetic procedures.

CA-III Year:
During the CA-3 year of training, residents are exposed to high-complexity cases in all anesthesia subspecialties, with unique opportunities in pediatric anesthesia, transplant anesthesia and difficult airway management. Furthermore residents will gain experience in practice management, non-operating room anesthesia and point-of-care ultrasound (PoCUS). Residents can select individual subspecialty rotations that best complete their training.
A complete list of rotations include:
- Advanced General Anesthesia
- Ambulatory Anesthesia
- Cardiovascular/Thoracic Anesthesia (CVT)
- Neuroanesthesia
- Advanced Obstetrical Anesthesia
- Surgical Critical Care (SICU)
- Neurosciences Critical Care (NSICU)
- Point-of-Care Ultrasonography (PoCUS)
- Non-operating Room Anesthesia (NORA)
- ENT/Difficult Airway
