-
Consultation-Liaison (C-L)
During their Consultation-Liaison (C-L) Psychiatry rotation, our residents gain hands-on experience with a wide range of psychiatric conditions in medically ill patients, from delirium and mood disorders to complex neuropsychiatric cases, all within the dynamic environment of a 600-bed tertiary care hospital. The C-L service works closely with multiple specialties including internal medicine, surgery, neurology, oncology, OB-GYN, and organ transplantation, providing consultations in general medical as well as intensive care units. This collaboration ensures that our residents receive well-rounded exposure to the critical intersection of psychiatry and medicine, learning to navigate the delicate balance of treating psychiatric symptoms in medically complex patients.
Our C-L service provides a truly multidisciplinary learning environment, where various levels of learners—psychiatry residents, neurology residents, addiction medicine fellows, and medical students—rotate through the service. This setup fosters a rich exchange of knowledge and perspectives, deepening the educational experience. Regular teaching rounds and case conferences are central to this process, offering structured opportunities for residents to engage with complex cases and learn from diverse viewpoints. The C-L psychiatry attending physicians are dedicated to providing personalized supervision and mentorship, guiding residents through challenging cases while encouraging independent decision-making and interprofessional collaboration.
Our C-L service supported by two dedicated teams, also hosts our Consultation-Liaison Psychiatry Fellowship Program (make the bolded into a hyperlink to the C-L fellowship website: https://www.rushu.rush.edu/education-training/graduate-medical-education/fellowship-programs/consultation-liaison-psychiatry-fellowship), providing residents with a unique opportunity to work closely with our C-L psychiatry fellow. This interaction adds another dimension to our residents’ education and growth.
-
MentorshipImage

At Rush, we believe that a strong mentor is an invaluable part of residency training. A mentor provides professional development and is key to helping trainees advance in their careers. Studies demonstrate that mentorships help enhance personal satisfaction of both trainees and faculty.
Each resident has an opportunity to get paired with a faculty mentor based on their specific interests, and can change or add mentors. The program leadership is available to help residents locate the right mentor, and to initiate meetings between the resident and their mentor. The program leadership routinely reviews mentorship experiences with each resident to ensure each mentor/mentee relationship is optimal.
Additionally, each PGY-1 gets paired up with a senior resident buddy. These buddies provide invaluable social and professional support to our interns as they transition into residency life.
-
Psychotherapy and PsychopharmacologyImage

Our program strives to teach residents to integrate both the psychopharmacological and psychotherapeutic paradigms in the assessment and care of patients that require psychiatric treatment. We have numerous attending psychiatrists who provide direct supervision to our residents. All PGY-2, PGY-3 and PGY-4 residents carry their own caseload of psychotherapy and medication management patients in the outpatient psychiatry clinic. They all participate in weekly psychodynamic psychotherapy and pharmacotherapy supervision and lectures. Additionally, PGY-2 and PGY-3 residents participate in weekly cognitive behavioral therapy (CBT) lectures and all PGY-3 residents receive weekly CBT supervision. Our PGY-2 residents sharpen their group therapy skills by rotating in the intensive outpatient program of our Road Home Program for veterans. Through hands-on training, supervision, and didactics, our residents gain extensive experience with the core psychotherapies. Over the past three decades, our curriculum has evolved into one of the most in-depth psychotherapy training programs in the Midwest.
-
Outpatient PsychiatryImage

The psychiatry residency has been designed to best reflect how most psychiatrists practice. Almost all psychiatrists practice some aspect of outpatient psychiatry. We have set up the curriculum to begin outpatient exposure in the second year and provide intensive outpatient psychiatric training during the third and fourth year of training. This gives residents the invaluable opportunity to work with the same patients for up to three years under expert supervision. Residents work with specialists in mood disorders, psychosis, women’s psychiatry, child psychiatry, geriatric psychiatry, and addictions.
Our Child and Adolescent team also works with local elementary schools to provide psychiatric and psychological services there.
Rush offers a range of outpatient services including neuromodulation (ECT, TMS, and esketamin - see below), telepsychiatry, a collaborative care clinic in internal medicine and pediatrics, a day hospital program, and specialty outpatient psychiatry clinics.
Our department offers electroconvulsive therapy (ECT), transcranial magnetic stimulation (TMS), and esketamine as valuable treatment options. Residents gain exposure to these treatment modalities as part of their Mixed Services Rotation in their second year. They can also devote elective time in their fourth year to develop expertise in these modalities.
Through our affiliation with Thresholds (a large community program that provides mental health services and housing, employment, and education resources to individuals with serious mental illnesses), residents are able to
- participate in their assertive community treatment (ACT) team to deliver psychiatric services directly in patients' homes, in homeless shelters, or on the street.
- perform true community outreach by joining Thresholds counselors in going to various neighborhoods to educate the lay public on medication-assisted treatment options
- take part in their Arrest Deflection Program and learn how Thresholds staff members partner with the 11th District of the Chicago Police Department to to divert individuals charged with substance use-related crimes out of the penal system and into the recovery system.
-
Collaborative Care
Rush offers the opportunity to participate in Collaborative Care Psychiatry during the PGY-2 year, as well as an elective during the PGY-4 year of training. Collaborative Care is a unique model that allows for the integration of behavioral health and medical services that has been shown to improve patient outcomes and reduce stigma related to mental health. Our residents work with their skilled supervisors who are double-boarded in Psychiatry and Internal Medicine. During their Collaborative Care rotation, residents collaborate with social workers and primary care physicians in an interdisciplinary model to provide efficient cost-effective mental health care for our patients. Many of our residents use this time to give presentations to primary care faculty and to publish scholarly reports with the supervisors.
-
Inpatient PsychiatryImage
Rush offers two adult inpatient psychiatric units on its main campus. This includes:
- an Adult Mood Disorders Unit
- a General Adult Psychiatry Unit
Having two distinct units enhances our ability to tailor treatment plans, including specialized group therapy, to the needs of each patient population.
All PGY-1 residents rotate on the two adult inpatient psychiatric units for half of the year. Our PGY-2 residents also rotate on the inpatient psychiatric units for one month. A PGY-4 inpatient chief resident supervises, teaches, and supports junior residents and students, and performs vital administrative tasks such as liaising between the junior residents, unit leadership, and residency program leadership. PGY-4 residents also have an opportunity to run an inpatient team as a junior attending.
Multidisciplinary Rounds (MDRs) are held every day on the inpatient psychiatric units. MDRs are attended by residents, attendings, nursing staff, unit administration, occupational therapists, and the case management team. These rounds facilitate strong discharge plans and collaboration between the various team members. They are an excellent platform to coordinate patient care, providing opportunities to collaboratively make changes to our patients' treatment plans and address any barriers to discharge. MDRs contribute to the high quality of care we provide to our patients.
-
Child and Adolescent PsychiatryImage

Residents spend a month of their PGY-2 year rotating in child psychiatry. This becomes an invaluable experience for residents choosing to fast track into child psychiatry as it gives them early exposure to the field before deciding whether to apply for fellowship. They have a choice between:- Assessing new patients in our ambulatory Child and Adolescent Psychiatry Clinic, performing inpatient psychiatric consultations for the pediatric population at Rush University Medical Center (RUMC), and child psychiatry consultations in the RUMC emergency department.
- Rotating on the inpatient child psychiatry unit at Garfield Park Hospital under the tutelage of their Chief Medical Officer (and graduate of our residency and fellowship programs).
Residents continue their training in their PGY-3 year, spending half a day a week in our Child and Adolescent Psychiatry Clinic. They maintain their own case load under expert supervision.
-
Road Home ProgramImage
 Image
Image
The Road Home Program: The National Center of Excellence for Veterans and Their Families at Rush is a nationally renowned program providing a range of outpatient mental health care services to our military veterans and their families. Funded in part by a $45 million grant from the Wounded Warrior Project, one of the largest gifts in Rush's history, the Road Home Program provides services free of charge to patients and their family members (adults and children alike) both locally and across the country. The Road Home Program boasts an impressive array of nationally recognized experts trained in military culture including trauma psychiatrists and psychologists, social workers, and traumatic brain injury specialists. It offers intensive outpatient programs for veterans suffering from post-traumatic stress disorder or military sexual trauma. It offers telepsychiatry to treat veterans in more remote areas once they complete treatment locally. It also uses virtual reality to provide graded exposure therapy in a therapeutic, supervised setting. All PGY-2 residents spend a month rotating on the Road Home program, actively working with a cohort of veterans in their intensive outpatient program.
-
Boot Camp
During the first 4-week block of internship year, all psychiatry residents rotate on the inpatient psychiatry units together. Over the past few years, this has received significant praise as it 1) eases residents' transition into residency, 2) allows all residents to get to know each other prior to being split into the traditional "psychiatry" block or "medicine" block, 3) gives residents more time to get to know the inpatient team (social worker, attendings, nurses, occupational therapists, mental health technicians) and electronic medical record system (Epic), and 4) permits more time to be devoted to didactics when beginning residency training in psychiatry
-
Substance Use Disorders InitiativesImage
 Image
Image
Rush University Medical Center has a strong emphasis on addressing the nationwide substance use disorders epidemic. Residents play a role in combating this epidemic through significant training in substance use disorders throughout their four years of residency. As PGY-1s and -2s, residents encounter and treat individuals with co-occurring disorders (i.e., a substance use disorder and another mental health disorder) during their hospital-based rotations, such as inpatient psychiatry, emergency psychiatry, and consult liaison psychiatry. During their PGY-2 year, residents spend a month rotating on the Substance Use Intervention Team (SUIT), a multidisciplinary inpatient consultation service that screens every patient admitted to Rush for problems with alcohol or other drugs. On this rotation, residents advance their knowledge of - and skills in - medication assisted treatment, motivational interviewing, and case management. During their PGY-3 year, residents spend half a day each week rotating in the Addictions Psychiatry Clinic. Most of our residents have also taken advantage of buprenorphine training programs in order to eventually obtain a license to prescribe this medication.
-
Rush University Medical CenterImage
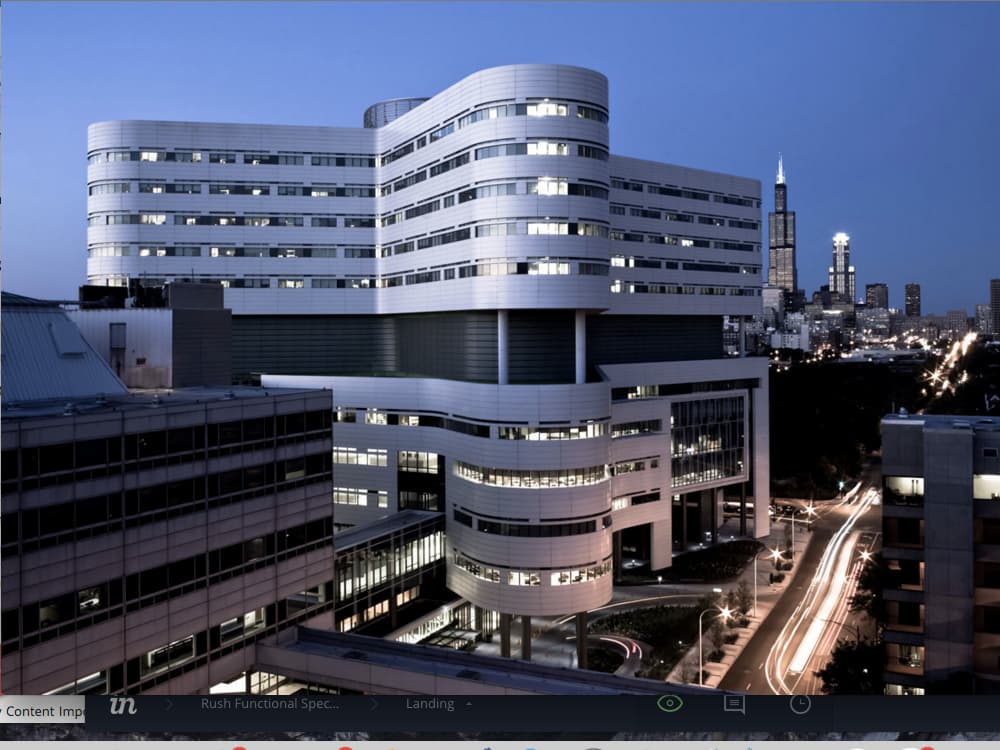
Our residents benefit from training in a strong academic department and also a state-of-the-art medical center. Rush University Medical Center offers outstanding residency and fellowship training in most medical specialties and sub-specialties. There are approximately 620 house staff per year. Rush Medical College trains approximately 520 medical students per year. The institution is widely recognized as one of the leading patient care hospitals in the nation and a center for academic excellence. Rush University Medical Center is located in the heart of one of the world’s greatest cities. Rush draws in a diverse, multicultural patient population from all socioeconomic backgrounds, significantly enhancing a resident’s training experience.
-
Moonlighting at Rush
Starting in their PGY-2 year, psychiatry residents have the opportunity to moonlight at Rush University in the evenings and on weekends. Moonlighting is voluntary and typically consists of seeing psychiatric consultations in the emergency department. In addition to serving as an extra source of income, moonlighting allows for additional clinical training under attending supervision, amongst familiar staff and colleagues.
-
Illinois Psychiatric SocietyImage

Residents have an opportunity to serve as representatives to the Illinois Psychiatric Society (IPS). Our residents, Drs. Josh Eloge and Alan Akira, won the IPS Resident of the Year Award in 2020 and 2021, respectively. Residents also have an opportunity to attend the Illinois Psychiatric Society Advocacy Day in Springfield, Illinois, residents gain exposure to how mental health laws are developed and how mental health resources are allocated. Residents have an opportunity meet with various state lawmakers to promote improved care of patients with mental health disorders, and to support the field of psychiatry.
-
Neuroscience Curriculum
With the assistance of our program leadership and the National Neuroscience Curriculum Initiative (nncionline.org), psychiatry residents Joshua Eloge, MD and Faraz Sultan, MD, PhD, developed and implemented an interactive, flipped classroom style neuroscience curriculum for PGY-1s through -4s. Residents interested in teaching have an opportunity to lead hour-long workshops and half-day symposia on the neuroscience of psychiatric disorders, from making brains out of Play-Doh to practicing how to discuss neuroimaging findings of borderline personality disorder to a patient.
2150 W. Harrison St.
Chicago, IL 60612
Phone: (312) 563-1212
psychiatry_residency@rush.edu
