Our innovative curriculum builds upon our Department’s unique characteristics. As one of the most up-to-date Emergency Departments in Chicago, we feel the clinical experience is unmatched and residents will graduate with all of the essential clinical skills required of an Emergency Physician. However, we offer several additional program features that will provide our graduating residents with skills that go above and beyond the clinical expectations of an Emergency Physician.
Didactics
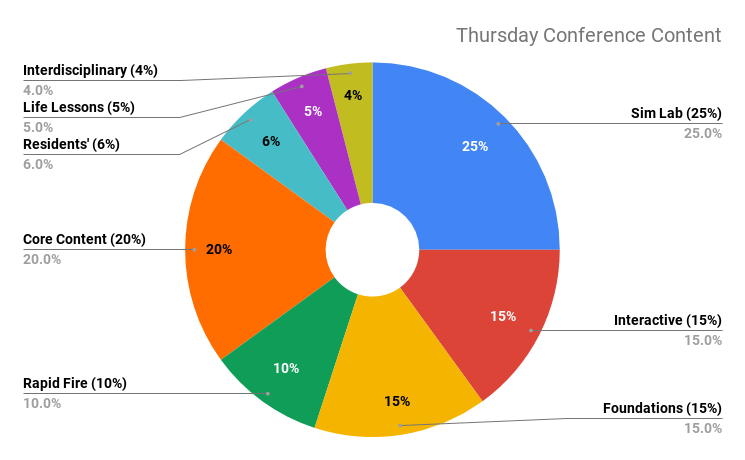
Each week, residents have 5 hours of protected learning experience. Conferences are high yield, interactive, and incorporate case-based and small group modalities as well as journal clubs, mock oral boards, and clinical case presentations. Both small and large group sessions are led by residents and our nationally recognized faculty. Some common themes include 5-minute EKGs and radiology, 5-minute Journal Club, M&M, EM Foundations, Quality Improvement, ultrasound, and simulation. Joint lectures with other RUSH departments as well as other Chicago-based EM programs, facilitate interdisciplinary and interinstitutional collaboration. The curriculum repeats every 18 months, thereby exposing residents to all of the expected material twice prior to graduation. Individualized independent instruction is managed through online learning platforms and an individualized faculty-coaching program.
Simulation
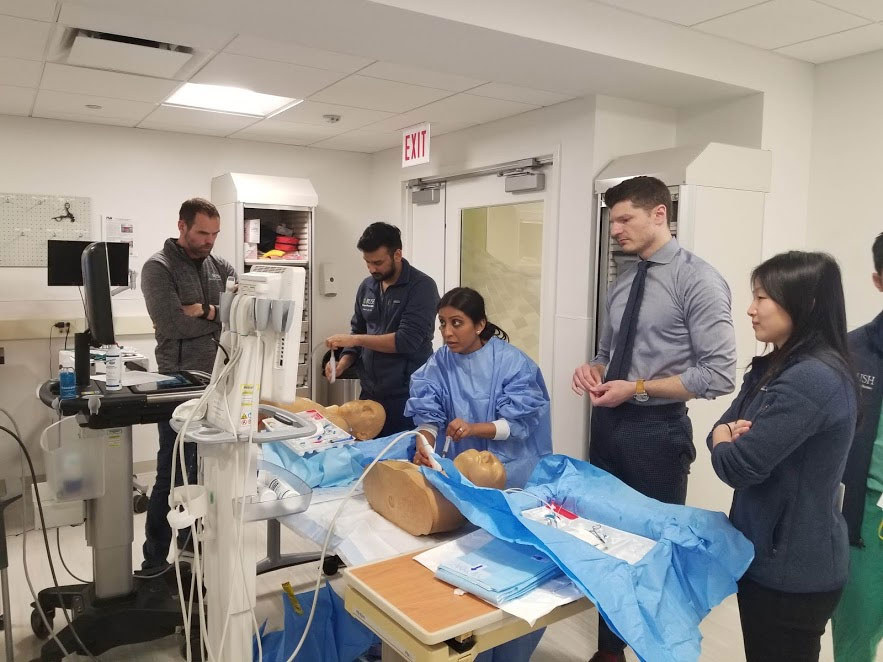
The RUSH Center for Clinical Skills and Simulation is a state-of-the art, multidisciplinary training center immediately adjacent to our departmental offices. We have one of the most immersive simulation experiences in the country, and spend over 25% of our didactic time in the sim lab. The RUSH Center for Clinical Skills and Simulation recently completed a major expansion. As one of the highlights of our program, it features real and simulated ED rooms with high-fidelity simulators, task trainers, and mass casualty environments. Simulation experiences occur in our clinical simulation lab, in situ in the ED, or as part of a procedural training exercise.
Director Dr. Sara Hock explains didactics at the RUSH Center for Clinical Skills and Simulation.
Health Equity
Our Division of Health Equity is one of the few such deliberately conceived programs in Academic Emergency Medicine. We value universal health care equitably accessible to everyone, and our Health Equity Division uses this principle to inform our patient care, training, advocacy, community partnerships, and scholarship. The Rush Department of Emergency Medicine recognizes that the structural inequities in our broken healthcare system are pervasive in our communities and are tragically visible in the Emergency Department. We are uniquely positioned to recognize structural racism and unequal social determinants of health. This compels us to effect change and reduce these disparities by approaching everything we do through the lens of health equity. We do this by:
- Programs: Our faculty demonstrate expertise in health justice, addiction medicine and substance use disorder, social emergency medicine, global health, trauma informed care, psychiatric emergencies and mental health access, community engagement, street medicine, interpersonal and sexual violence, immigration and asylum health, and health equity informatics. Our programs include inpatient and outpatient substance use intervention teams, trauma-informed care programs, and immigration health outreach programs for asylum seekers.
- People We invest in training the next generation of health equity experts, and support our faculty engaged in this work. Our training programs include fellowships in Health Equity and Social Emergency Medicine, Behavioral Health Emergencies, and Addiction Medicine. Our residency training program specifically teaches social and global medicine and anti-racism practices. Our faculty teach community-based CPR, medical student programs in health justice, and mentor students at all levels who come from backgrounds considered to be underrepresented in medicine.
- Policies: Our departmental policies start with addressing questions of health equity. Our team screens for social determinants of health from the moment of arrival throughout their ED stay, and strives to connect patients with resources that matter. Our department works to identify our own biases and disrupt racist policies that prevent our patients from achieving the health they deserve.

EMS & Disaster Preparedness
RUSH EM Residents train in a state-of-the-art disaster hospital built for mass causality events and a global pandemic. Intentional and longitudinal experiences are available in the hospital Haz-Mat team as well as resident-leaders of the Rush Advanced Trauma Training Program, an educational program that teaches EMTs and Paramedics from the military pre-hospital trauma essentials. Rush residents have opportunities to partner with Rush 911, a collaborative community-based Rush Medical College student group focused on teaching Chicago-land community members bystander CPR, Stop-The-Bleed, as well as Narcan training for opioid overdose. Residents are encouraged to participate in event medicine and opportunities to medically volunteer in local events are accessible. Rush EMS-fellowship trained faculty offer research projects, an elective, and opportunities to further their interest in EMS. For more information about EMS exposure during your Residency at Rush, contact nicholas_cozzi@rush.edu
Quality Improvement
Residents learn the skills and language of quality improvement through an integrated program of self and peer assessment. From the first month, residents are integrated into the department’s quality improvement process. Residents are assigned to teams to review intubations, ICU upgrades, ED unscheduled returns, and focused case reviews. Through mentorship by faculty and senior residents, teams learn to identify quality indicators and patient safety. The teams work together to support senior level presentations and many residents expand on these experiences to develop quality improvement projects that have made significant impacts to operations in the RUSH Emergency Department.

Diversity
RUSH University Medical Center believes that equal opportunity and diversity in employment, education, and the delivery of health care are essential and must be furthered.
Living this mission statement is fundamental to our program, and our residents and attendings are active members of RUSH's Diversity, Equity, and Inclusion Committee. Residents are given subsidized opportunities to travel to professional development programming, such as the annual SNMA Medical Conference. RUSH Emergency Medicine is also happy to offer our scholarship for the Rush Diversity and Inclusion Visiting Scholars Program (VSP). VSP seeks exceptional medical students who have demonstrated a commitment to health equity and addressing health and healthcare disparities in underserved and marginalized communities.

Women in Medicine
RUSH is home to the Center for the Advancement of Women in Healthcare, an incubator and advocate for gender equity in all levels of our nation’s healthcare workforce. More than 50% of the ED faculty are women, and overall 40% of RUSH’s leaders are women, and 45% of RUSH’s residents and fellows are women. The RUSH Women in EM is a group of ED attendings and residents working to amplify one another and advocate for gender equity in the medicine, career advancement, and work-life balance. The group hosts a bimonthly lunch series, live speakers, and wellness events. RUSH faculty include the founder of the All-Chicago Women in EM Group, which meets frequently for networking, lectures, and social events. Members are active participants in the FeminEM Idea Exchange (FIX) conference and Women in Medicine (WIM) Summit.

Social & Global Emergency Medicine
The Social EM & Global Health resident track is an optional course for RUSH EM residents interested in learning more about social determinants of health, global health issues, and social programs to improve the lives of our immediate community. The group often hosts live speakers who are involved with research, volunteerism, or advocacy groups locally and globally to accompany relevant online coursework. RUSH EM residents also provide in-country support to emergency physicians in the Dominican Republic through established teaching programs in toxicology, ultrasound, simulation, and EMS. Locally, our residents are involved in neighborhood outreach, pipeline programming, and gun violence advocacy.

Journal Club
Every other month, our Journal Club meets for an evening of dinner, drinks, and a critical review of key publications pertaining to topics of our choice. Some recent topics have included low-risk chest pain clinical decision tools, TPA in acute stroke, management of tachyarrhythmias, and pharmacologic therapy for influenza.
Want to learn more? Check out our videos and webinars on the "How to Apply" page.
