Each year of residency consists of 26 two-week blocks. All residents will have four weeks of vacation taken annually in 1 two-week block and 2 one-week blocks. Below is a general outline of the schedule of intern and senior residents.
PGY-1 Residents
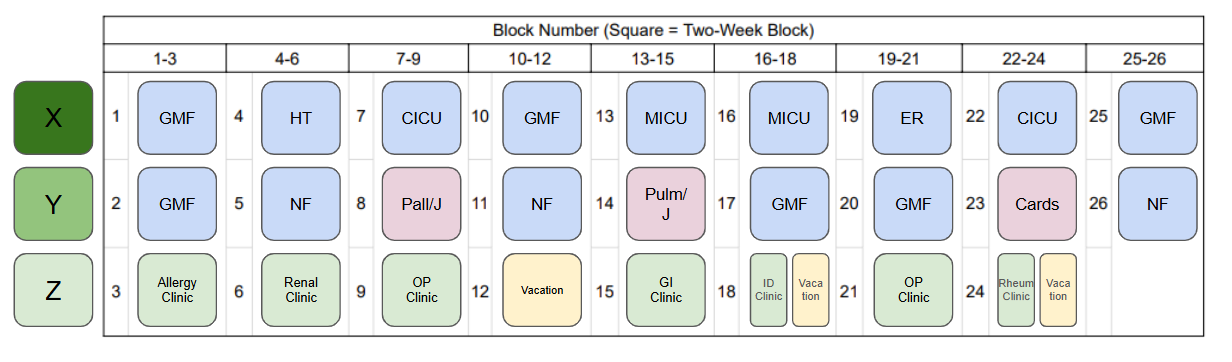
- 12 weeks of general medicine
- 6 weeks of night float
- 4 weeks of medical intensive care unit (MICU)
- 4 weeks of cardiac intensive care unit (CICU)
- 2 weeks of inpatient hematology teaching service
- 4 weeks of subspecialty consult services
- 12 weeks of outpatient medicine
- Split between primary care and subspecialty clinics
- 2 weeks of palliative/pain management
- 2 weeks of emergency medicine
- 4 weeks of vacation
The image to the right is an example of a hypothetical intern schedule
PGY-2 Residents
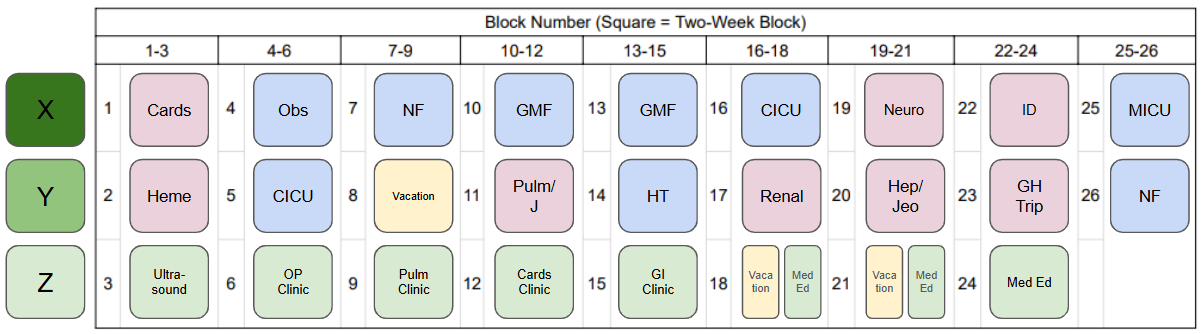
- Approximately 20 weeks of inpatient service (general medicine floors, medical ICU, cardiac ICU, night float, malignant hematology service) per year
- 12-18 weeks of inpatient consults
- 2 weeks of the observation unit
- 2 weeks of general/stroke neurology consults
- 12 weeks of outpatient medicine
- Split between primary care and subspecialty clinics
- 4 weeks of vacation
- Electives: subspecialty consult services and subspecialty clinics, including an HIV consults rotation at Stroger
- Dedicated block time for research, global/community health, quality improvement, or medical education projects
The image to the right is an example of a hypothetical PGY-2 schedule.
PGY-3 Residents
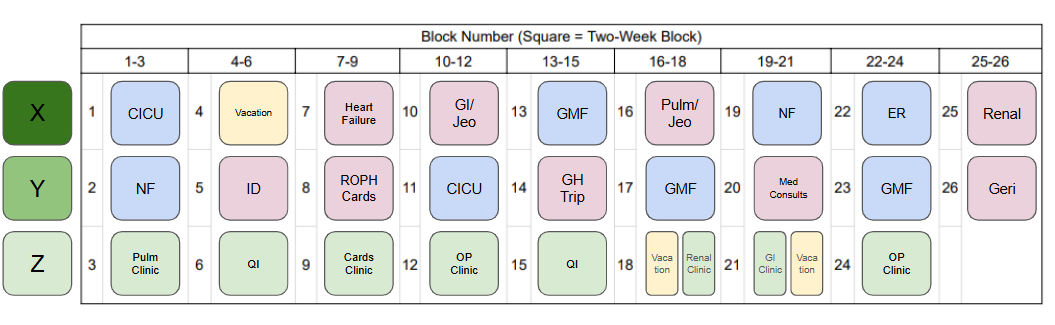
- Approximately 16 weeks of inpatient service (general medicine floors,
medical ICU, cardiac ICU, night float, malignant hematology service) per year - 2 weeks of medicine consult service
- 2 weeks of geriatric medicine
- 2 weeks of emergency medicine
- 12 weeks of outpatient medicine
- Split between primary care and subspecialty clinics
- 4 weeks of vacation
- Electives: subspecialty consult services and subspecialty clinics, including an HIV consults rotation at Stroger
- Dedicated block time for research, global/community health, quality improvement, or medical education projects
The image to the right is an example of a hypothetical PGY-3 schedule.
Outpatient experiences
All categorical interns have a primary care continuity clinic that occurs during their outpatient (OP) block. Residents have the option of choosing between the following primary care clinics:
- RUSH University Internists
- Community Health site (CHC)
- CHC is the largest volunteer-based free clinic in the nation with a focus on providing a medical home at no cost to low-income, uninsured adults.
The remainder of our residents’ outpatient blocks consist of clinics in the Internal Medicine subspecialties, including cardiology, gastroenterology, pulmonary, hematology, oncology, and nephrology clinics. Other outpatient electives include sports medicine, ophthalmology, and dermatology.
Didactics
Intern Didactics: A dedicated curriculum for the interns, intern didactics consists of a mix of both case based and lecture style reports, developed over years to introduce interns to important foundational topics in medicine in an informal environment.
Resident Report: RUSH believes in a “residents as teachers” model in which our residents deliver presentations on Mondays and Tuesdays. Residents work with the Chief Residents in advance to become the best teachers they can be. The talks themselves are moderated by a Chief Resident and an Attending Physician.
Noon Conference: This conference takes place on Thursdays and Fridays and is led by an Attending Physician or Fellow Physician, covering both interesting topics in medicine as well as issues that are often under-represented in medicine, such as health inequity, resident finances, artificial intelligence, and more.
Internal Medicine Grand Rounds: Hosted every Wednesday, presented by RUSH faculty or invited guest speakers. Topics range from specialized and innovating procedures to multidisciplinary case conferences.
Internal Medicine Board Review: Hosted throughout the second half of the academic year as part of the noon conference lecture series
Outpatient Didactics: During their outpatient blocks, residents receive outpatient-focused didactics during an academic half day. These small-group discussions include talks from primary care physicians, subspecialists, and non-physician experts to give residents a well-rounded outpatient educational experience.
Point of Care Ultrasound (POCUS) Curriculum
All internal medicines will participate in a longitudinal ultrasound curriculum throughout their residency. Four sessions occur throughout each year in the simulation center. These sessions include didactics, image review, hands-on practice with standardized patients, and procedure training using ultrasound guidance.
Sessions are taught by faculty and fellows in the Pulmonary/Critical Care Division and cover the following topics:
- Cardiac ultrasound/echocardiography
- Lung ultrasound and thoracentesis
- Vascular ultrasound and central venous catheter placement
- Abdominal ultrasound and paracentesis
Senior residents can apply to participate in an ultrasound elective. This elective includes the following:
- Hands-on experience with point of care ultrasound in the intensive care unit daily, guided by Pulmonary/Critical Care faculty and fellows
- Sessions with echocardiography technicians to improve image acquisition
- Training with advanced practice nurses experienced in placing peripherally inserted central catheters and ultrasound guided peripheral IV placement
- Asynchronous teaching sessions on advanced ultrasound techniques
- Opportunities for educational and clinical research on ultrasonography
