The three-year ACGME-accredited Neonatal-Perinatal Medicine Fellowship Program at RUSH University Medical Center (RUMC) fully meets the requirements of the Neonatal-Perinatal Medicine subspecialty board of the American Board of Pediatrics. The program provides trainees with a broad range of experiential clinical, research, teaching and leadership opportunities, with the goal of training physicians who achieve excellence in all four domains. The 72-bed, state-of-the-art level 3 (highest designation in Illinois) single family room Neonatal Intensive Care Unit (NICU) provides specialized interdisciplinary, neonatal care that is family-centered and evidence-based. Training occurs as a continuum, with progressively more clinical responsibility and dedicated research time over the three-year fellowship experience. Most clinical activities are conducted at RUMC, a large tertiary-care academic hospital and referral center in Chicago. Fellows also spend two weeks in the Rush Copley NICU for a community hospital experience. Fellows rotate at the Ann & Robert H Lurie Children’s Hospital, an affiliate of RUMC, for their Cardiac ICU rotations and one Maternal-Fetal Medicine rotation.
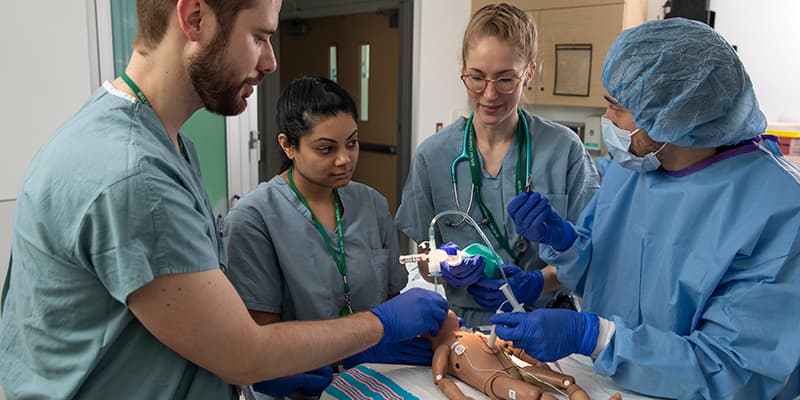
Clinical training is evidence-based, with direct patient care, didactic and hands-on simulation-based components. Fellow responsibilities include patient care, consultation with specialists/sub-specialists, antenatal counseling, parent/family conferences, transports, in-house night call, and collaboration with the interprofessional healthcare team to provide optimal care for patients in the NICU. Clinical NICU training comprises 13 months of the three-year Program; 5.5 months in year one, 4.5 months in year two and 3 months in year three. In addition to overseeing the management of patients in the NICU, in collaboration with advanced practice providers, fellows serve as supervisors for house staff, junior fellows and medical students.
-
Year 1
During the first two weeks, fellows are oriented to the NICU environment, and program expectations are outlined. Fellows participate in neonatal resuscitation training (NRP), simulation-based complex conversations training, a ventilator workshop and the Midwest Neonatal Simulation Boot Camp, as well as other onboarding activities. During the first year, each fellow spends a total of 5.5 months in the NICU. Under the direction of an Attending neonatologist, fellows are expected develop skills required to diagnose and provide clinical care, gain experience in neonatal resuscitation and delivery room management, and coordinate transports. Fellows are expected to gradually gain skill in common neonatal procedures and begin to develop teaching and leadership skills, progressing throughout the first year. Fellows achieve an increasing level of responsibility and independence, based on demonstrated ability and confidence as they progress throughout the year.
Weeks Rotation 2 Orientation/Simulation-based training 22 NICU 4 Maternal-Fetal Medicine 2 Radiology 18 Research 4 Vacation - Maternal-Fetal Medicine: Fellows rotate with the Maternal-fetal medicine service to understand and participate in the care of families with high-risk pregnancies and those with morbidities that can impact the fetus. During the rotations fellows participate in interdisciplinary consultations for parents/families with high-risk/complex pregnancies in the Rush Fetal-Neonatal Medicine Center clinic and the Chicago Institute for Fetal Health at Ann & Robert H. Lurie Children’s Hospital.
- Radiology: The two-week rotation is designed to provide one-on-one training with a pediatric radiologist for fellows to learn the interpretation of neonatal radiologic studies, including x-rays, CTs, ultrasounds, MRIs, etc.
-
Year 2
In the second year, each fellow spends a total of 4.5 months in the NICU, and the second year builds upon the first. With progressively less direct supervision, fellows are expected to demonstrate increasing knowledge of fetal/neonatal physiology and pathophysiology, develop diagnostic and treatment plans, direct and supervise clinical care, and demonstrate developing skill in neonatal resuscitation and delivery room management. Fellows are expected to conduct transports and demonstrate more advanced procedural and teaching ability. As the second year progresses, fellows are expected to demonstrate emerging leadership skills and attain growing knowledge of the administrative aspects of the field of neonatology.
Weeks Rotation 18 NICU 4 Pediatric Cardiac ICU 24 Research 4 Vacation - Pediatric Cardiac ICU: To gain an understanding of congenital heart defects and experience in the pre- and post-operative management of neonates with congenital heart defects, fellows rotate (in year 2 and 3) with the cardiothoracic teams in the Pediatric Cardiac ICU at Ann & Robert H. Lurie Children’s Hospital. Fellows also participate in a four-day, interdisciplinary hands-on ECMO training course at RUMC.
-
Year 3
During the third year, each fellow spends a total of 3 months in the NICU. Third-year fellows are expected to function with increased independence, and for the final two clinical rotations function as the “Acting Attending Physician” (under the supervision of the Attending Physician on service). Fellows are expected to apply advanced knowledge of neonatology to develop diagnostic and treatment plans and direct and supervise the interprofessional care team, demonstrate procedural proficiency and advanced clinical and leadership skills in neonatal resuscitation and delivery room management. Third year fellows are responsible for teaching and supervising house staff, junior fellows and students. The third year provides fellows the opportunity to develop advanced leadership skills and additional knowledge and experience in the administrative aspects of neonatology.
Weeks Rotation 12 NICU 4 Cardiac ICU 32 Research 4 Vacation

High-Risk Follow-Up Clinic
Fellows rotate in the RUSH Neonatal High-Risk Follow-Up clinic during their research rotations. Fellows work closely with the Attending Neonatologist and the multidisciplinary team that includes neurodevelopmental child psychologists, dietitians and physical therapists. Fellows participate in the longitudinal evaluation and management of high-risk neonates, including very low birth weight infants, those who received therapeutic hypothermia and those with congenital heart disease.
For questions about the program and/or application process:
Beverley Robin, MD, MHPE, CHSE, FAAP
Program Director
Beverley_Robin@rush.edu
(312) 942-6640
Kathryn L. Lindsey
Program Coordinator
Kathryn_L_Lindsey@rush.edu
(312) 942-8311
ACGME program ID: 3291632099
