Because it works. Evidence shows that interprofessional experience helps health workers gain the skills needed for practice-ready jobs.
In both clinical practice and education, interprofessional education encourages a focus on teamwork based not on a specialty or hierarchy, but rather on effectiveness and outcomes aimed at bringing together everyone who works with patients.
What does interprofessional education teach us?
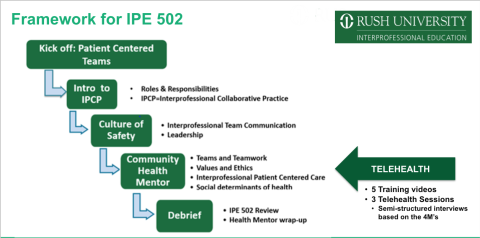
Our interprofessional education efforts follow core competencies set out by the International Education Collaborative to ensure students have the knowledge, skills and values they need to function as part of a team and to provide effective patient-centered collaborative health care. These core competencies are as follows:
- Values and ethics: Work in an ethical and respectful manner with all members of the health care team responsible for investigating, developing and delivering patient-centered health care
- Roles and responsibilities: Engage diverse professionals to complement one’s own professional experience
- Communication: Communicate with clarity, confidence and respect in encouraging ideas and opinions of other team members to ensure a common understanding of information, treatment and health care decisions
- Teams and Teamwork: Apply leadership practices that support collaborative practice, team effectiveness and patient-centered health care

Mission & Vision
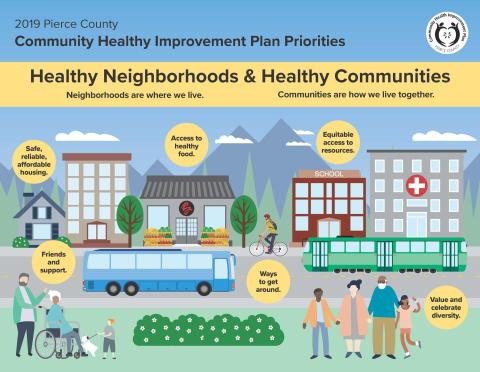
Mission: The Office of Interprofessional Education advances patient-centered, collaborative learning and impactful scholarship, which fosters a culture of inclusion that promotes the health and well-being of our diverse communities.
Vision: The Office of Interprofessional Education will be an internationally recognized driver of innovative, experiential education, committed to instilling a collaborative culture to prepare a practice ready workforce that promotes the well-being of our diverse communities.
Through our office, you can access a variety of interprofessional courses and advanced student interprofessional learning opportunities.
Get a glimpse of Ahrianna's experience in IPE 502
IPD 502 Community Health Mentors share their experience.
For more information on interprofessional education at RUSH University, please contact:
Jan Odiaga, DNP, CPNP-PC
Director, Office of Interprofessional Education
Associate Professor, College of Nursing
ipe@rush.edu